How CAR NK therapy works
With CAR NK therapy clinical trial, natural killer cells live up to their ominous name
An experimental treatment called CAR NK therapy finally helped B-cell lymphoma patient JC Cox overcome cancer after years of trying different options. Now, researchers are exploring how to expand this treatment to more cancer patients and cancer types.

JC Cox knows the meaning of perseverance. In fact, he embodies it after undergoing a dozen different cancer treatments, including a CAR NK therapy clinical trial.
The first sign of trouble occurred in 2006. JC, who had always worked long hours as an air conditioning and heating technician, began to lose steam.
“I’d come home after work and fall into bed immediately without eating dinner,” he recalls. “The next thing I knew, it was morning, and I was still exhausted.”
But the hardworking JC soldiered on, until one day, he could barely breathe.
“I tried to inhale but couldn’t,” he says. “That’s when I sounded the alarm and headed for the emergency room.”
A follicular lymphoma diagnosis
In the hospital, doctors discovered that lymph fluid had built up in JC’s chest cavity and spilled into one of his lungs, causing it to collapse. They drained 5 gallons of the excess fluid from his body, then sent it to the lab for analysis, along with tissue from a swollen lymph node.
JC was stunned when the results came back. His diagnosis? Follicular lymphoma, a slow-growing type of cancer that affects B cells – the white blood cells that circulate in the lymphatic system and battle infections.
“I thought I’d caught a virus,” says JC, now 66. “Cancer never crossed my mind.”
After absorbing the news, JC and his wife, Kathy, vowed to fight.
“No way were we going to back down,” Kathy says. “We were prepared to do whatever it took.”
We were prepared to do whatever it took.
Initial follicular lymphoma treatments
JC’s treatment began with six cycles of chemotherapy at a Dallas hospital near his home. That put him in remission for 13 months, but the cancer came back. He then endured three more rounds of high-dose chemotherapy. It wiped out not only his cancer cells, but also many of his healthy blood cells, making him vulnerable to infection.
“We were warned this would happen,” Kathy says. “The healthy cells become collateral damage in the battle against cancer – it’s just part of the process.”
To replenish the healthy cells that chemotherapy had destroyed, JC underwent a stem cell transplant. Immature cells that would later develop into healthy blood cells were collected from his bone marrow and infused back into his bloodstream. The treatment worked for four months, but, again, the cancer returned.
Seeking lymphoma treatment at MD Anderson
Out of options, JC’s Dallas doctor referred him to MD Anderson. Here, he might be eligible for a clinical trial of an immunotherapy drug called ipilimumab, trade name Yervoy. The drug trains the immune system to find and attack cancer cells. But in some patients, the drug also attacks healthy cells, causing serious side effects.
That’s exactly what happened to JC. He ran a high fever, fell into a coma and ended up on life support.
“Finally he recovered, and we were so relieved,” recalls Kathy. “But my husband was in desperate need of better options.”
At that point, Sattva Neelapu, M.D., professor of Lymphoma and Myeloma, prescribed a drug named Rituximab. It didn’t eliminate the cancer, but it did prevent it from spreading – for a while. In 2017, JC’s follicular lymphoma transformed into diffuse large B-cell lymphoma, a more aggressive form of the disease. He endured several aggressive chemotherapy treatments, but they only kept the cancer at bay a few weeks at a time.
“I had tumors on my face and my temples that came back every two weeks after chemo,” JC recalls. “It was a race, and the cancer was winning. We had to do something quickly.”
CAR T cell therapy clinical trial wasn’t an option
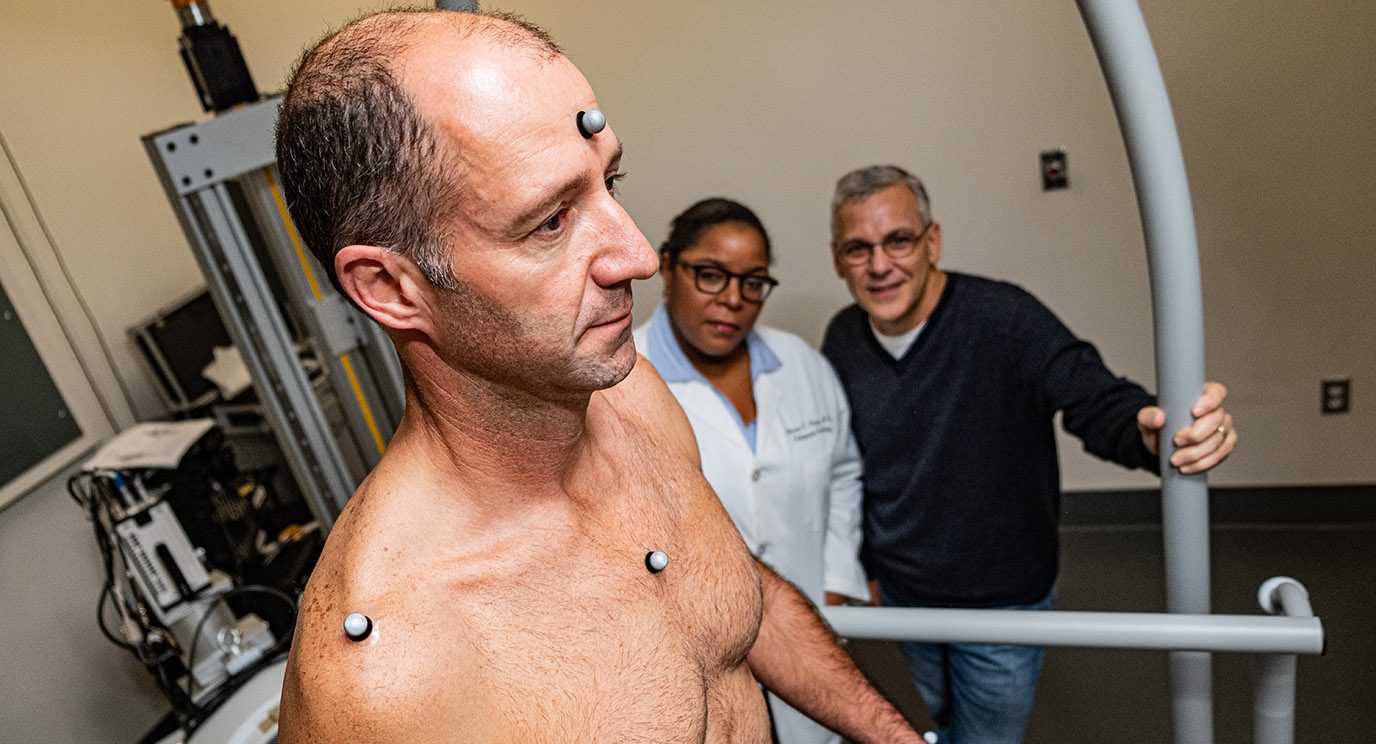
By then, JC was on the waiting list for a clinical trial of a groundbreaking new cancer treatment called chimeric antigen receptor (CAR) T cell therapy. Disease-fighting T cells are extracted from the patient’s blood and taken to the lab, where scientists infuse them with a special receptor named CAR that binds to certain proteins on cancer cells. Large numbers of these CAR T cells are multiplied in the lab, then infused back into the patient’s body to seek out, stick to and kill cancer cells. CAR T cell therapy achieved approval from the Food and Drug Administration (FDA) while JC was still on the waiting list. This meant the clinical trial no longer needed to accept new patients.
“That was bad timing,” he recalls, “and very disappointing to hear.”
CAR NK cell therapy clinical trial offers hope
Just when it looked like JC options were again dwindling, a new clinical trial testing CAR NK therapy was launching at MD Anderson.
Similar to the recently approved CAR T cell therapy, the new clinical trial would add CAR to natural killer cells, also called NK cells. These disease-fighting cells live up to their ominous name by lurking in the body and being the first to respond to damaged or stressed tissues. They are capable of recognizing and killing cancer cells.
“NK cells are very good at recognizing cancer cells early on and destroying them, but cancers can develop ways of hiding from the immune system,” says Katy Rezvani, M.D., Ph.D., a professor of Stem Cell Transplantation and Cellular Therapy. “By engineering NK cells to include CAR, we’re able to expand upon their innate cancer-killing abilities.”
Multiple doses of CAR NK cells can be manufactured from one donor. These can then be used to treat multiple patients.
Because of their unique properties, CAR NK cells have the potential to be manufactured in advance, frozen and stored, and made immediately available for any patient in need.
The bounceback from my treatment was amazing.
Finally cancer-free, thanks to CAR NK therapy clinical trial
JC enrolled in the clinical trial and became only the eighth person in the world to be treated with CAR NK cells.
Just 30 days later, while analyzing his follow-up scans, Rezvani told JC that things looked “pristine.” That was April 2018, and he’s been cancer-free ever since then.
The results of the clinical trial that JC participated in were published in the New England Journal of Medicine in February 2020. Rezvani and her team treated 11 patients in the clinical trial with CAR NK cells.
Seven, including JC, achieved complete remission, meaning all signs and symptoms of cancer had disappeared. One had a partial remission, meaning evidence of cancer decreased, but did not completely disappear.
“While this is a small study and our follow-up is relatively short, we are extremely pleased with the promising results,” says Rezvani. “We will continue to investigate CAR NK cells in broader clinical trials, and we hope that this will be an effective new treatment option for many patients in need.”
The therapy caused no significant side effects – another advantage of CAR NK cells.
“The bounceback from my treatment was amazing,” says JC. “It was like I didn’t even get sick. I was embarrassed to walk the halls at MD Anderson because I felt so good.”
We hope that this will be an effective new treatment option for many patients in need.
A second stem cell transplant
With all signs of cancer gone, JC underwent a second stem cell transplant in August 2018, to get his beleaguered body in fighting shape, on the off-chance the cancer came back. His brother Gary was a perfect match, so he traveled to Texas from his home in Maryland to donate stem cells.
“We’ve always been tightknit,” JC says, “but this takes closeness to a whole new level.”
After the transplant, JC visited Rezvani every month for checkups. As time went by, the intervals between his visits became longer – first three months, then six. Today, he sees Rezvani once a year.
Expanding CAR NK therapy to treat more cancers
In November 2019, MD Anderson announced a new license and research agreement with Takeda Pharmaceutical Company to develop and advance CAR NK cell therapies. This strategic partnership is critical to bringing CAR NK cells to more patients through multi-institutional trials, which will determine whether CAR NK cells will become an FDA-approved treatment.
Today, Rezvani and her team are working to expand CAR NK cell therapy to 10 additional types of cancer. She hopes to bring the next generation of CAR NK cells into the clinic as quickly as possible.
JC is hopeful as well, after seeing the benefits firsthand.
“Of all my cancer treatments, CAR NK cell therapy was by far the easiest,” he says. “We’re almost afraid to let our guard down, but I trust in Dr. Rezvani.”
Rezvani and her team led the development of CAR NK cells at MD Anderson, with the support of the adoptive cell therapy platform, the Chronic Lymphocytic Leukemia Moon Shot® and the B-Cell Lymphoma Moon Shot® , all part of MD Anderson’s Moon Shots Program® , a collaborative effort to rapidly develop scientific discoveries into meaningful clinical advances that save patients’ lives.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.