FAST clinic gives anaplastic thyroid cancer patients hope – and time
Historically, anaplastic thyroid cancer patients have had few treatment options, and those that existed often came too late. But MD Anderson’s FAST clinic is speeding up the start of treatment for this aggressive cancer – and giving patients new treatment options, including clinical trials.

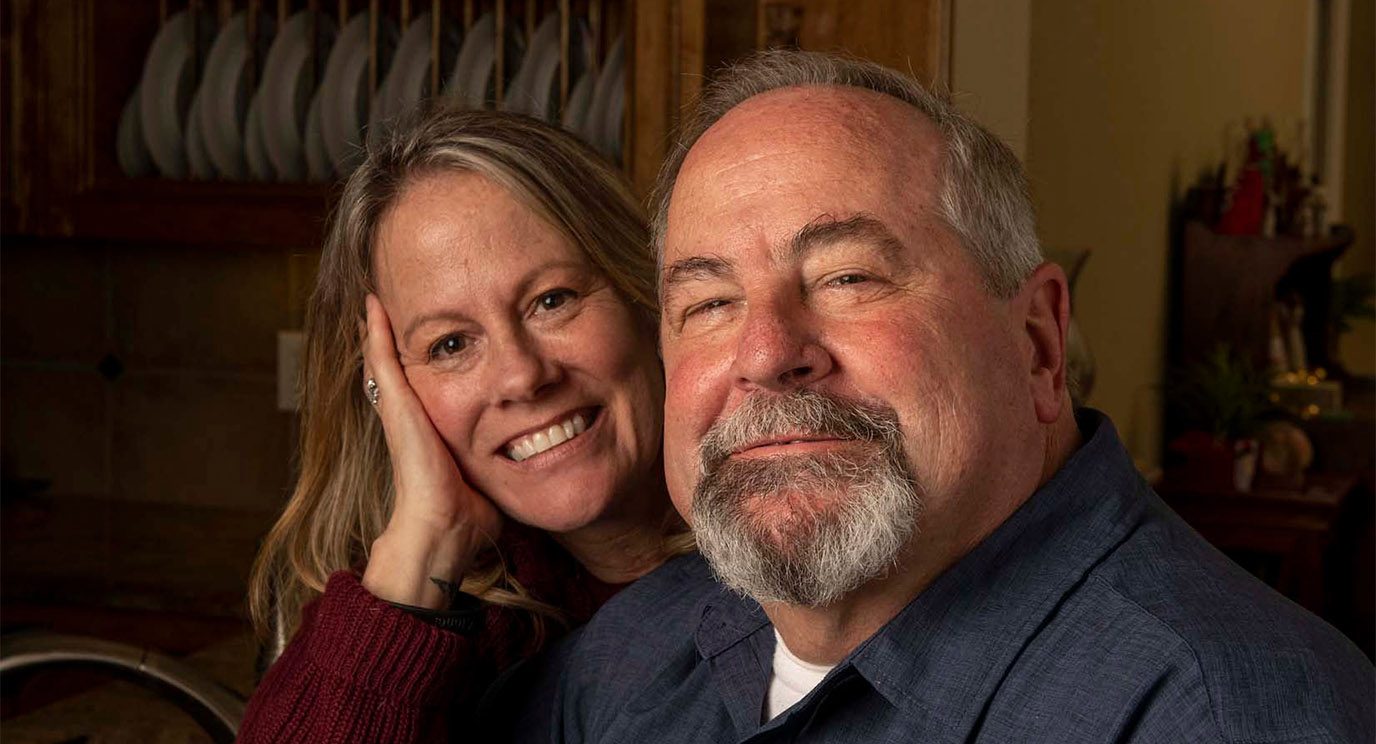
Max Nickless says he “wasn’t too optimistic” when his wife, Becky, drove him 15 hours from their home in Indiana to see thyroid cancer specialist Maria Cabanillas, M.D., at MD Anderson in February 2017. The outlook from local doctors was so poor that he’d already picked out photos and music for his funeral.
Max had anaplastic thyroid cancer – the most aggressive form of the disease. “Anaplastic” is a medical term used to describe cancer cells that divide rapidly.
“Anaplastic thyroid cancer is probably one of the deadliest human cancers,” says Stephen Lai, M.D., Ph.D., professor of Head and Neck Surgery. It’s rare – only about 1,000 cases per year in the U.S. – and most patients die within three to six months after diagnosis.
“When I talked to Dr. Cabanillas on Wednesday, Max was still eating and drinking, and everything was normal,” Becky says. “But by Saturday, he had trouble swallowing, a lot of trouble breathing, and I was really worried about driving him to Houston.”
The cancer’s rapid progression wasn’t unusual. Anaplastic thyroid cancer is so aggressive that by the time many patients are fully evaluated, their disease is often beyond help. Or at least, that’s the way it used to be.
Thankfully, Max’s diagnosis came at a time of historic progress in anaplastic thyroid cancer treatment.
Fast help for anaplastic thyroid cancer treatment
Several years earlier, Cabanillas and her colleagues took on the Herculean task of improving outcomes for anaplastic thyroid cancer patients.
“At that time, we really had nothing to offer them that they couldn’t get at home,” says Cabanillas. “What a disappointment, as a patient, to come to the nation’s No. 1 cancer center and be told to go get chemotherapy at home. We wanted to change that.”
Working with MD Anderson’s Clinical Safety and Effectiveness program, the team first identified doctors in Endocrinology, Medical Oncology, Radiation Oncology and Surgery who could devote special appointment slots in their clinic schedule each week to anaplastic thyroid cancer patients.
The FAST (Facilitating Anaplastic thyroid cancer Specialized Treatment) team was established in 2014, with a committed group of oncologic endocrinologists, medical oncologists, a radiation oncologist, a pathologist, a pulmonologist, and a head and neck endocrine surgeon. The group would work to get patients into treatment faster.
The streamlined system worked. The time to schedule an appointment for new anaplastic thyroid cancer patients dropped from 8.7 days to half a business day by 2018, Lai says.
We learned a lot about how to design clinical trials that are specifically for anaplastic thyroid cancer.
Targeted therapy clinical trial drug shrinks his tumors
Creation of the FAST team coincided with the opening of a clinical trial for several rare cancer types that involved a specific mutation in the BRAF gene. The mutation, known as BRAF (V600E), may increase the growth and spread of cancer cells. Max’s tumor had that mutation.
The international trial, led by Vivek Subbiah, M.D., associate professor of Investigational Cancer Therapeutics, was testing dabrafenib and trametinib, a targeted therapy combination that already had success treating melanoma in patients with a BRAF mutation. Targeted drugs block the growth and spread of cancer by interfering with specific molecules that help cancer progress.
Unfortunately, like most targeted therapies, the drugs were in pill form. Since Max couldn’t swallow by the time he got to MD Anderson, he didn’t quality for the clinical trial. Doctors came up with an alternative. Although Max wasn't in the trial, he would still get the drugs. He received his first dose of dabrafenib through a feeding tube.
“I remember asking Dr. Cabanillas when I would know if the dabrafenib was going to help. She said I would know within two days,” Max recalls.
He and Becky didn’t wait in Houston to find out.
“Becky was trying to get me home before I passed away so the kids could see me,” Max says. “That was our main concern.”
Two days later, Max realized he’d regained the ability to swallow when he started craving a soda on the drive back to Indiana. The dabrafenib was working as quickly as Cabanillas had predicted. Max’s tumor continued to shrink, and he began receiving trametinib about a month later.
A new anaplastic thyroid cancer treatment option
More than half the anaplastic thyroid cancer patients who qualified for the clinical trial saw their tumors shrink. In May 2018, the Food and Drug Administration approved dabrafenib and trametinib for anaplastic thyroid cancer patients with the BRAF (V600E) mutation. It was the first drug therapy ever approved to treat the disease.
“We learned a lot about how to design clinical trials that are specifically for anaplastic thyroid cancer,” Cabanillas says.
For example, a later trial allowed other drug delivery methods for patients who couldn’t swallow.
A high rate of clinical trial participation for anaplastic thyroid cancer patients
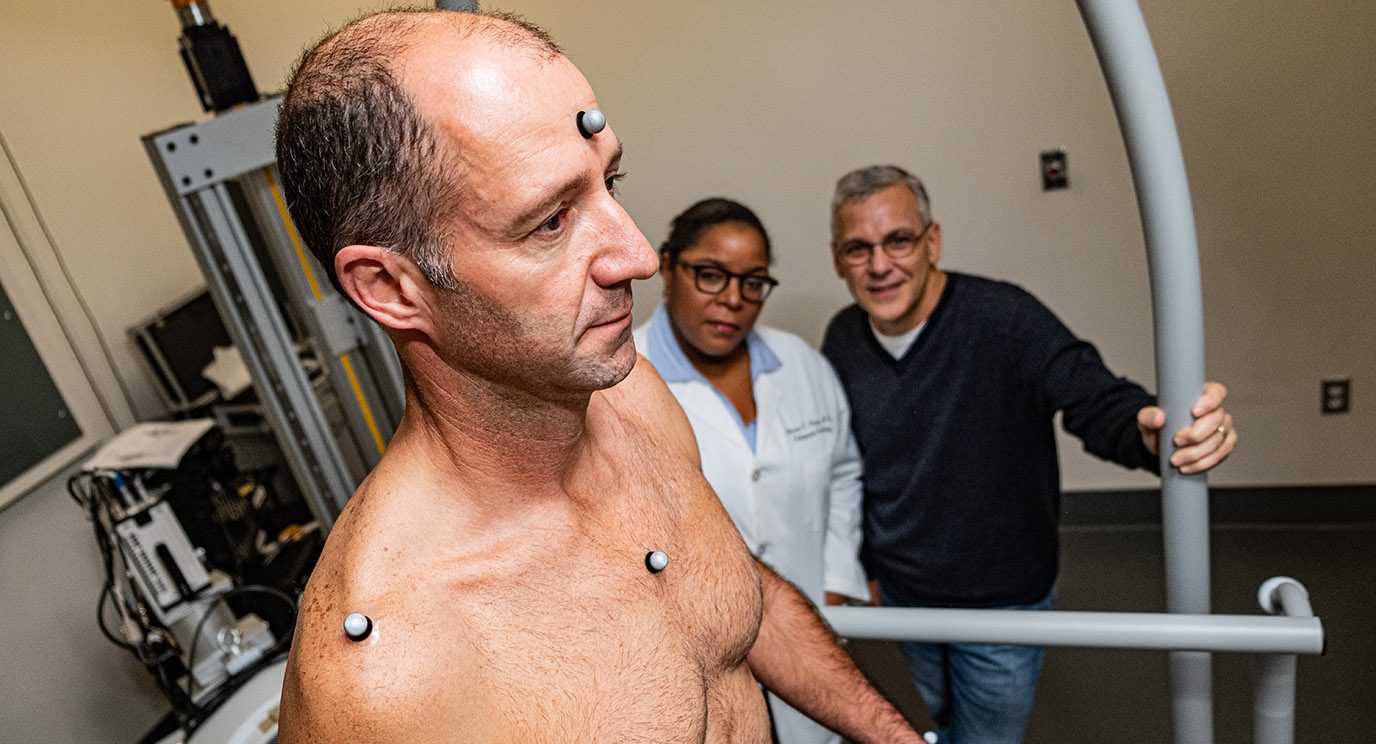
Thanks to the FAST team, more than 30% of anaplastic thyroid cancer patients at MD Anderson now enroll in clinical trials. One reason clinical trial enrollment is so much higher than the national average of 3% to 5% is MD Anderson’s use of a liquid biopsy, or blood test, that looks for mutations in cancer cells that are circulating in the blood. The goal is to target these mutations with drugs specifically designed to attack them.
“Traditionally, a tissue biopsy is taken from a patient’s tumor, then analyzed in the lab for mutations. The results often take weeks to come back, and these patients can’t wait that long,” says Jennifer Wang, M.D., assistant professor of Head and Neck Surgery. “Now, we’re able to order the liquid biopsy. Results usually come back within a week, which allows us to choose targeted drugs within a reasonable time frame.”
This is a paradigm shift.
Combating targeted therapy resistance
Some tumors treated with the targeted therapy combination that Max received eventually grow back, a problem known as resistance. When it became clear that Max’s tumor was starting to grow again, his doctors added the immunotherapy drug pembrolizumab to his treatment plan. Immunotherapy drugs train a patient’s own immune system to attack cancer.
Max’s care team hoped the immunotherapy would help control his tumor growth, but they didn’t stop there. They knew that when patients responded well to targeted therapy, their tumors shrunk enough to be removed with surgery – something that was almost never done before for anaplastic thyroid cancer.
“Traditionally, these tumors have been non-operable because they involve critical structures in the neck, such as the carotid artery or voice box,” says Mark Zafereo, M.D., associate medical director of MD Anderson's Endocrine Center. “But once patients had such a dramatic response to targeted therapy, we realized we could re-introduce surgery into the multidisciplinary care model and improve survival while still preserving quality of life. Surgeons have been historically reluctant to operate on anaplastic thyroid cancer patients because the prognosis has historically been so bad, so this is a paradigm shift.”
Zafereo successfully removed Max’s entire tumor in May 2017. Max then underwent 30 doses of radiation therapy. He stopped taking pembrolizumab in September 2019. Today, he remains cancer-free. He welcomed his fifth grandchild in February 2020, three years after his diagnosis.
We’re always trying to change the status quo.
Giving anaplastic thyroid cancer patients more time
In the August 2019 cover article of the journal Thyroid, MD Anderson published the first case studies to show that treating BRAF-mutated anaplastic thyroid cancer with dabrafenib and trametinib, followed by surgery and radiation, was safe and effective. In November, the team presented survival data during the Annual Meeting of the American Thyroid Association. Average overall survival at MD Anderson for anaplastic thyroid cancer doubled after the FAST team formed, from eight months in 2000-2013 to 16 months in 2017-2019, with more than 40% of patients surviving at least two years.
With the launch of MD Anderson’s Rare Tumor Initiative, which aims to identify additional molecular and genetic targets for the next generation of therapies for rare tumors, and two new clinical trials for anaplastic thyroid cancer opening soon, the team hopes to continue improving the care, survival and quality of life for all patients diagnosed with this once hopeless disease.
“At MD Anderson, how cancer is treated is constantly evolving. We’re always trying to change the status quo,” Wang says. “We want to lead and do everything possible to change the trajectory for these patients.”
Request an appointment at MD Anderson online or by calling 1-855-419-4861.