Back in the game after a brain tumor in the bladder
An unusual diagnosis of a brain tumor in the bladder was no match for the treatment planned by MD Anderson’s experts – or for University of Oklahoma soccer player Jazzy Richards.

As a soccer player for the University of Oklahoma, Jasmine Richards is used to being in the spotlight. But now she’s making headlines for another reason. “Jazzy,” as friends and family call her, is the only known person in the world to be diagnosed with a brain tumor in her bladder.
“She’s completely unique,” says Ashish Kamat, M.D., Jazzy’s doctor and a professor of Urology at MD Anderson. “A type of tumor that normally develops in the lining of the brain originated in her bladder instead. This just doesn’t happen.”
A perplexing cancer diagnosis
Jazzy’s cancer story began in summer 2018, when she collided with another player on the field during soccer practice. Shortly afterward, her back began to hurt, and she noticed blood in her urine. That’s when she sought medical attention at an Oklahoma hospital.
At first, emergency room doctors presumed Jazzy had a bruised kidney. But a CT scan revealed a small mass in her bladder – perhaps a blood clot, doctors thought. But when a urologist biopsied the suspicious tissue and sent it to a lab for analysis, the results that came back were troubling – and perplexing.
Jazzy had cancer, the report said, but it didn’t look like bladder cancer anyone had seen before.
“It looked unusual under the microscope, and they weren’t even certain it was bladder cancer,” Jazzy recalls. “Something wasn’t adding up.”
The hospital referred Jazzy to a urologist, who jotted down names of three top cancer centers in the country and told her to pick one. She chose MD Anderson in Houston because it’s near her parents’ home and is ranked first in the nation for cancer care.
I was on a mission. I wanted a road map for what to do next.
Seeking a road map for treating a brain tumor in the bladder
Kamat, who specializes in complicated cases, was taken aback when Jazzy arrived at his clinic.
“She was only 18 years old,” he says. “The average bladder cancer patient is 70.”
Kamat performed another biopsy. Once again, pathologists – this time at MD Anderson – were puzzled. Their analysis revealed the tumor was an ependymoma, an aggressive type of cancer that forms in the lining of the brain. So why was it in Jazzy’s bladder?
“I’d never heard of this before, and neither had our pathologists. But maybe someone else had,” says Kamat, who is president of two groups – the International Bladder Cancer Group and the International Bladder Cancer Network, whose members are the top physicians and scientists in the field. “I was on a mission to find a doctor who’d treated a patient with Jazzy’s same diagnosis. I wanted a road map for what to do next.”
He first queried MD Anderson’s brain tumor specialists, but none had ever seen a case like Jazzy’s. Next, he contacted specialists at major cancer centers across the country, then around the world. Every time, the answer was the same: ependymomas don’t occur in the bladder.
The hypothesis: “Drift” explains the brain tumor in her bladder
“Hundreds of the world’s leading bladder and brain cancer experts put their heads together, but we were all left scratching our heads,” Kamat says. “No one had encountered a brain tumor in the bladder.”
The group carefully considered how this could have happened. They arrived at what Kamat says is the only logical explanation: a phenomenon in the field of anatomy known as “drift.”
Here’s how it happens: All newly developing humans begin as a single cell resulting from the fusion of a female egg and a male sperm. In the uterus, this lone cell divides again and again into multiple cells, with each one destined to become a specific type – for example, a bone, cardiac or lung cell. The cells then migrate to their intended location where they help build organs and structures in the body.
“Perhaps one of Jazzy’s cells that was meant to become a brain cell mistakenly went to the bladder, where it hung around, mutated and became cancerous,” Kamat says. “It’s the only hypothesis that makes any sense.”
If Jazzy were my daughter, I’d want to do all I could to give her the best chance for a future.
No precedent for treating a brain tumor in the bladder
Scientists have documented cases involving drift throughout history, but no one had seen a case like Jazzy’s. Bottom line: Kamat was navigating in unchartered territory. With no prior knowledge to draw upon, he had no way of knowing what treatments would and wouldn’t work for his first-of-a-kind patient.
“We have well-established ways of treating commonly occurring cancers,” Kamat says. “But in Jazzy’s precedent-setting case, we didn’t have that advantage.”
He met with Jazzy and her parents, Carolyn and Walter Richards, and proposed two options: Monitor the tumor, and if it grows, remove the entire bladder to prevent the tumor from spreading. Or, remove the bladder now.
“If Jazzy’s tumor had developed in her brain, we know it would have behaved very aggressively,” Kamat explains. “Surgical removal would be the only way to treat it. Chemotherapy wouldn’t work, because ependymomas are generally chemo-insensitive.”
But Jazzy’s tumor was in her bladder, not her brain, so perhaps it would behave differently. Kamat considered removing the tumor while leaving her bladder in place. But after intense discussions with colleagues, he dismissed the idea.
“That’s a gamble we weren’t willing to take,” Kamat says. “What if the tumor grew back and spread quickly?” he says. “We’d be out of options.”
He thought about his daughter, who is close in age to Jazzy.
“If Jazzy were my daughter, I’d want to do all I could to give her the best chance for a future,” he says. “I’d remove the bladder.”
Jazzy and her parents agreed without hesitation.
“Jazzy can live without a bladder,” says Carolyn, “but we can’t live without Jazzy.”
I wanted to have the best chance of continuing to play soccer and the lowest possibility of the cancer coming back.
Weighing the treatment options
Now the Richards family faced yet another decision. Once Jazzy’s bladder was removed, Kamat could build her a new one using tissue from her small intestine. Or, Jazzy could do without a bladder and wear an external pouch called a urostomy bag for urine collection.
The first option – constructing a new bladder – is one of the most complicated surgeries performed at MD Anderson, Kamat says.
“Think of the bladder as a balloon,” he explains. “The round, inflatable part of the balloon is the bladder where urine is stored. The balloon’s mouthpiece is the bladder’s neck. This neck connects to the urethra, a tube that carries urine out of the body.”
If Jazzy decided on a new internal bladder, Kamat would need to remove her old one but leave the neck of her original bladder in place. He’d then hook her new, man-made bladder up to her old bladder neck.
This could invite trouble, Kamat cautions.
“Cancer cells from Jazzy’s original tumor could be lurking in the neck of her original bladder,” he explains. “There’s a risk these cells could spread into her new bladder.”
And there’s one more downside: Jazzy would need to train her new, man-made internal bladder to function properly.
“It takes about seven to eight months to train a replacement bladder,” Kamat says. “You’re like a toddler going through toilet training. You have accidents.”
Jazzy turned down the internal bladder, choosing the external bag instead.
“I wanted to have the best chance of continuing to play soccer and the lowest possibility of the cancer coming back,” she says. “If that meant wearing a urostomy pouch, then that was the choice I felt was best.”
Back in the game
Once Jazzy made her treatment decision, it was “off to the races,” Kamat says.
“She was focused and determined. I told her, ‘It’s just like soccer. I’m the coach, you’re the player. Listen to me and follow my instructions. We’ll do this together.’”
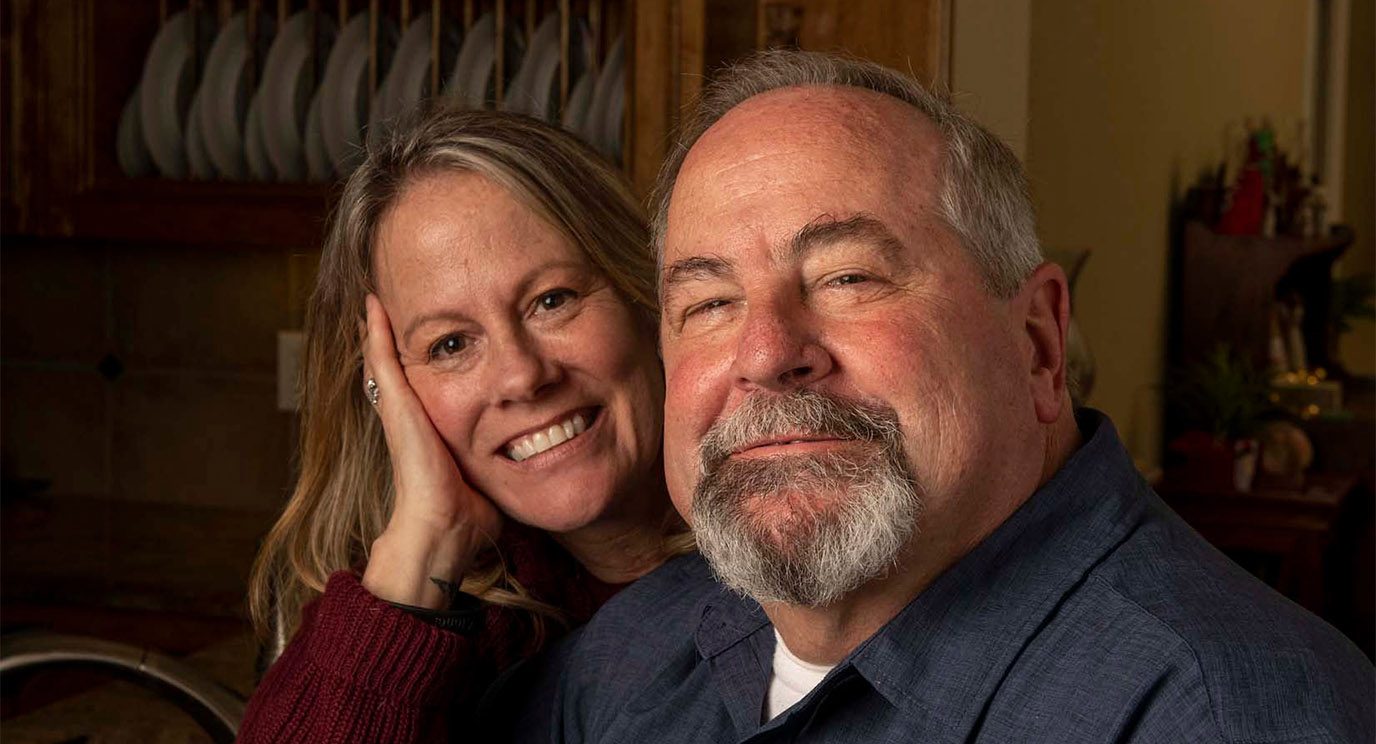
Jazzy was the perfect patient. Six weeks after her surgery was completed by Kamat and a team of reconstructive surgeons, she returned to school. Her flawless 4.0 grade point average never faltered.
Little by little, she became stronger as she followed Kamat’s guidelines about how to build up her endurance.
When soccer season began last August, she was back on the field. Carolyn watched from the stands and cried tears of joy when her daughter scored her first-ever goal against The University of Texas.
“Cancer sidelined Jazzy most of her freshman year. Not participating was hard for her,” Carolyn says of her daughter, who in high school scored more points and goals than any other player in her school’s history and was named Most Valuable Player in her district.
Today, a year after surgery, Jazzy is cancer-free. She visits MD Anderson every three months for checkups. As time goes by, she’ll return less frequently. Eventually, she’ll be seen once a year, then every other year.
We all listened and learned from each other.
Team approach enabled successful treatment of one-of-a-kind patient
“Should another patient someday be diagnosed with a brain tumor in the bladder, their health care team can look to Jazzy’s case for treatment guidance,” Kamat says.
He applauds the multidisciplinary team of MD Anderson experts who weighed in on Jazzy’s case, including pathologists, neuro-oncologists, urologists and others. Providers from multiple disciplines met to discuss Jazzy’s case when she was first admitted, recalls John de Groot, M.D., professor of Neuro-Oncology.
“We all listened and learned from each other,” he says. “Then, we developed a treatment plan we believed would work best.”
“It’s a tremendous advantage to have experts from all different fields working together at one institution to care for a patient,” Kamat says.
Now I know I can handle anything that’s thrown my way.
Looking ahead
Now a sophomore accounting major, Jazzy says she “gives thanks every day” for her health care team. She’s happy to be back among friends and focusing on the future.
“I believe in staying grounded and taking life in stride, but this experience really challenged me,” she says. “Now I know I can handle anything that’s thrown my way.”
Request an appointment at MD Anderson online or by calling 1-888-925-3903.