Real-time support for newly discharged patients and caregivers
The hours and days after hospital discharge can be overwhelming. Now, askMDAnderson is ensuring cancer patients and caregivers get the help they need when they need it.

A recently discharged patient said he was feeling fine when nurse Liliana Larsson called to check on him. But as Larsson asked more questions, the patient said he was light-headed, seeing white spots and couldn’t get a reading from his blood pressure monitor.
As a care manager for askMDAnderson, Larsson has the clinical training and people skills needed to ask the right questions. She’s part of a new clinical team that helps patients continue to benefit from MD Anderson’s care after they’ve gone home.
All patients discharged from the hospital, Emergency Center, and outpatient surgical and procedural areas receive automated phone calls within 24 hours. The calls start with a recorded greeting from Chief Nursing Officer Carol Porter, D.N.P., before transitioning to a short automated survey about their care, how they’re feeling and whether they have questions about discharge instructions and medications.
Twelve care managers, who are trained registered nurses and advanced practice registered nurses, monitor responses and answer patients’ requests within a day. They document calls electronically so the patient’s care team has the up-to-date information needed to help the patients the next time they’re seen.
It can be hard to remember care instructions when you have so much on your mind.
Easing caregiving and recovery at home
Many patients have questions and concerns about drains, ports, medication and pain. They want to know if something’s normal or a sign to seek medical attention.
“It can be hard to remember care instructions when you have so much on your mind,” Larsson says.
Care managers ask for details so they can pull out information to help patients manage their symptoms. Larsson and her teammates use resources such as patients’ electronic health records and MD Anderson’s online education materials to help patients be informed.
“We have an obligation to provide patients with the support they need, when they need it,” says Elizabeth Garcia, associate vice president of Patient Experience. “Immediately following discharge can be a vulnerable time for patients and their family members, so we have to be proactive and responsive.”
Garcia says it’s important to help patients get to an emergency room quickly when needed, or if appropriate, give them additional information to help them manage their care at home.
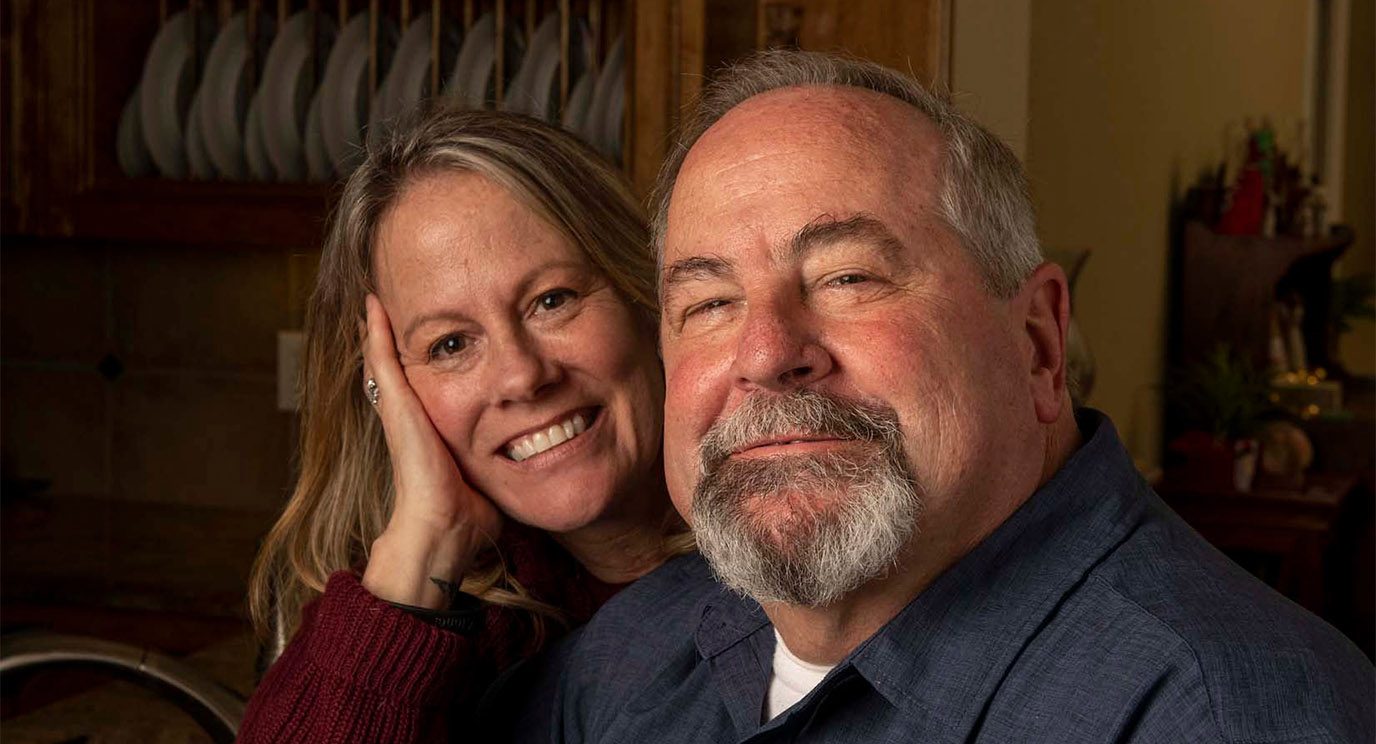
In the case of the patient who was seeing spots and failing to get a blood pressure reading, Larsson encouraged his caregiver to seek immediate assistance, and the patient arrived by ambulance safely at a hospital in his town. However, Larsson recounts an exchange with a caregiver who called repeatedly because he was anxious about managing his wife’s care correctly.
“He gave me updates, and I told him he was doing a great job,” Larsson says. “And then I encouraged him to get some sleep and take care of himself so he could continue to take great care of her.”
Without Larsson’s advice, both the patient and caregiver might have spent hours worrying at home or waiting to ask a question in an emergency room.
Their help is valuable in ensuring patients’ questions are answered.
Real-time support benefits cancer patients and their providers
Since the team started in August 2019, more than 40,000 discharged patients have received automated calls, and more than 26,000 patients have received answers to questions about their care.
Janice Finder, director of Patient Experience Clinical Services, says the high number of responses from the patients called shows they’re engaged in their care. She says things can change when patients go home, so other clinicians appreciate that care managers provide real-time support.
The number of after-hours pages to providers has dropped by 48% since care managers started helping patients, says Michael Frumovitz, M.D., associate chief patient experience officer.
Joanna-Grace Manzano, M.D., assistant professor of General Internal Medicine, is grateful that care managers listen carefully to every detail.
“Their help is valuable in ensuring patients’ questions are answered, and if needed, they quickly reach out to the right provider for additional guidance,” says Manzano.
Research shows interventions like these elevate quality and continuity of care by reducing unnecessary Emergency Center visits and unplanned hospital readmissions, says Chief Patient Experience Officer Randal Weber, M.D. They also lower an organization’s overall cost of care and protect the time and capacity of emergency rooms and hospitals to care for their most critical patients.
“This means a safer, more efficient, less expensive and more satisfying care experience for patients,” Weber says.
Support even after clinic hours
Any patient with a clinical question who calls MD Anderson’s main line and askMDAnderson during evenings, weekends and holidays can speak with a care manager directly. Care managers document everything and only page providers if needed. During the day, patients with clinical questions are connected with their clinics.
A nurse for 15 years, with more than seven years at MD Anderson, Larsson knows how busy care team members can be. She says supporting patients and care teams makes this her most rewarding role ever.
After-hours support is available by calling 1-877-632-6789 Monday through Friday from 5 p.m. to 11 p.m. and Saturday, Sunday and holidays from 8 a.m. to 7 p.m.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.