A new approach to monitoring blood transfusion patients
MD Anderson’s first-of-its kind Hemovigilance Unit is enabling care teams to virtually monitor cancer patients before, during and after a blood transfusion. That means quicker detection, response to and prevention of blood transfusion reactions.

In a continued effort to provide patients with the best care, MD Anderson has developed a first-of-its-kind Hemovigilance Unit to virtually monitor cancer patients before, during and after a blood transfusion.
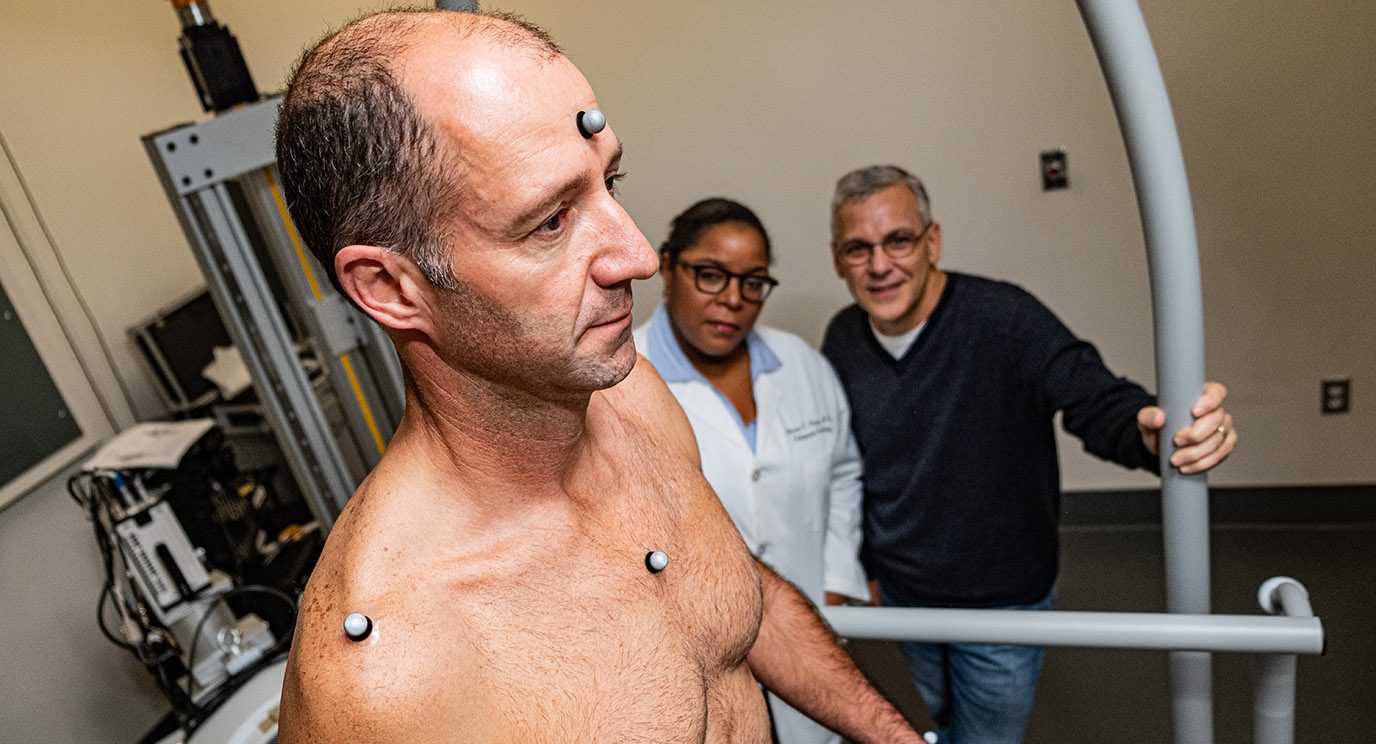
The Hemovigilance Unit (HVU) is a collaborative effort between the Nursing, Laboratory Medicine and Information Technology departments that brings cancer patient care, transfusion medicine and technology together in an innovative way.
“We were looking at how to better identify transfusion reactions and respond in a meaningful manner,” says James Kelley, M.D., Ph.D., assistant professor and laboratory director in Laboratory Medicine, who co-leads the HVU with Dee Gallardo, executive director for Nursing.
The concept of a centralized virtual hub for patient monitoring is not new to medicine. Hospitals have had cardiac telemetry units that allow for continuous monitoring of patients’ hearts for decades. However, it was Carol Porter, D.N.P., chief nursing officer and senior vice president for Nursing, who envisioned using the concept for blood transfusion monitoring at MD Anderson.
“Giving a transfusion to a cancer patient is a different treatment because their bloodwork is different. They may not react the same as a person who doesn’t have cancer,” says Porter.
Cancer treatment’s side effects can often mirror the warning signs of an adverse transfusion reaction, making reactions more difficult to identify in cancer patients. Porter and her team saw this as an opportunity for MD Anderson to lead the way in detecting, responding to and preventing transfusion reactions.
There’s so much more data.
Team approach enables quick response for blood transfusion patients
To develop this unprecedented team approach, nurses and transfusion specialists worked with computer engineers to design an intuitive tool capable of sorting through patient data to identify high-risk patients and to offer real-time support to frontline staff. Using this tool, the Hemovigilance Unit can inform a care team about a patient’s transfusion-related risks before, during and after a blood transfusion, so they can intervene, if necessary.
“There’s so much more data. You’re not one nurse with one patient,” explains Porter. “There’s a whole group that’s connected.”
An on-call unit of nurses and advanced practice providers is able to remotely monitor vitals of every transfusion patient at MD Anderson’s Texas Medical Center Campus, as well as our locations in The Woodlands, West Houston, League City and Sugar Land. If a patient shows any sign of an adverse reaction, the unit can send a practitioner to the patient’s bedside quickly.
“If the Hemovigilance Unit nurses take note of an increase in a patient’s transfusion reaction score and there’s a suspicion of a transfusion reaction, they’ll contact their advanced practice provider HVU colleague, who deploys to the patient’s location, if warranted. When on the scene, the advanced practice provider speaks with the primary nurse, evaluates the patient, and also collaborates with the primary advanced practice provider or attending physician to render care,” explains registered nurse and certified nurse practitioner Tonita Bates, who supervises the Hemovigilance Unit’s staff of specially trained nurses and advanced practice providers.
“When caring for patients, you need as much support, as much reinforcement and as many eyes as you can, and that’s what the Hemovigilance Unit does. It allows our outstanding nurses to have this invisible backup helping to monitor and manage what is happening,” adds Rosanna Morris, MD Anderson’s chief operating officer, who oversees inpatient and outpatient operations.
Us being at our best means that we are that much closer to ending cancer.
Data provides new insights to manage blood transfusions, improve patient care
The specialized unit oversees between 20 and 200 patients each day. Blood transfusions are the most common inpatient procedure at MD Anderson. Last year, the center transfused more than 190,000 blood products, or about 1% of the nation’s total transfusion procedures. Using the data collected and analyzed by the Hemovigilance Unit, the large number of transfusions at MD Anderson will now offer scientists new insights into transfusion medicine.
By collecting data on the different factors that may possibly impact the success of a blood transfusion, researchers can analyze and identify new variables that may influence an adverse reaction.
“Once we know those patterns, and that structure is figured out as an algorithm, every time a patient receives a transfusion, we can put all the new variables into the system and in real-time be able to predict which patients may or may not have a reaction,” says Kelley. “We’re actually building artificial intelligence models around these data so that we can build a human-machine hybrid.”
The Hemovigilance Unit’s success and the data it offers have the potential to “impact patients, potentially worldwide, on a safer way to give blood products,” says Porter. “We are creating – as a team and as a hospital – a new standard.”
Morris agrees.
“The Hemovigilance Unit is yet another example of the great work, the great research and the great innovation that has come from MD Anderson,” she says. “Us being at our best means that we are that much closer to ending cancer. And that’s what this team is all about.”
Request an appointment at MD Anderson online or by calling 1-866-915-2971.