Are you at high risk for pancreatic cancer?
A new clinic to identify and monitor those at high risk for developing pancreatic cancer continues to expand after opening last year.

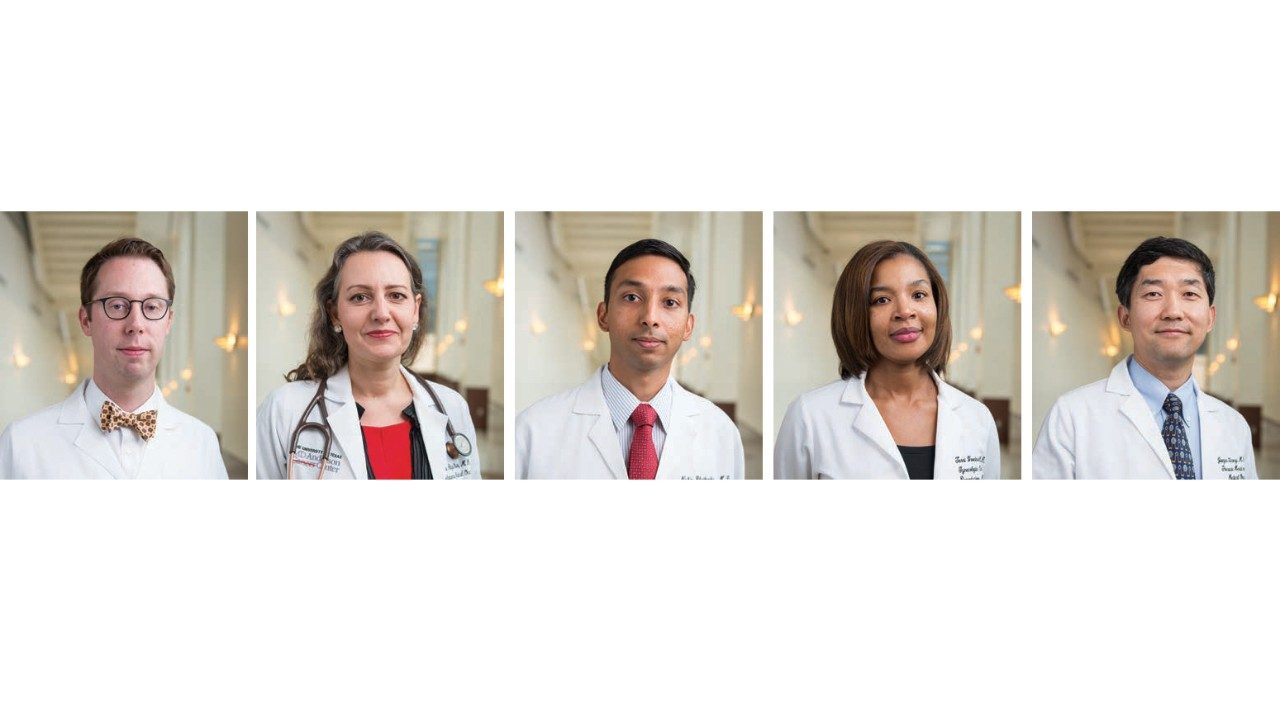
The clinic’s goal is to find ways to detect the disease early, when a cure may be possible, says its director, Florencia McAllister, M.D., assistant professor of Clinical Cancer Prevention.
“Due to the location of the pancreas, early tumors can’t be seen or felt by health care providers during routine physical exams,” McAllister says. “Patients are usually diagnosed when the cancer cannot be surgically removed.”
Who’s at risk?
Pancreatic cancer risk is higher in those whose parents, siblings or children developed the disease, particularly at a young age, and in those who have any of 10 genetic mutations, including a mutation in the BRCA2 gene, better known for raising breast cancer risk.
Family history coupled with genetic mutations place a person in the high-risk category. Some genetic mutations alone place a person at an increased risk, even without a family history of pancreatic cancer. One example is a mutation in the STK11 gene, which can be found in people with Peutz-Jeghers Syndrome. The syndrome causes noncancerous growths in the gastrointestinal tract and puts people at a greatly increased risk of developing certain types of cancer, including cancer of the gastrointestinal tract, pancreas, cervix, ovaries and breast.
Other factors such as chronic inherited inflammation of the pancreas, called pancreatitis, are powerful and well-known risk indicators.
At MD Anderson’s high-risk clinic, patients are tested for a blood biomarker called CA-19-9, which can indicate cancer but also is prone to false positives. Magnetic resonance imaging and endoscopic ultrasound examinations follow, McAllister says.
Clinic participants are relatives of MD Anderson patients, referrals from other clinics, such as breast, or self-referrals — usually relatives of cancer patients.
Recent studies have found that about 1% of adult patients diagnosed with new-onset diabetes will also be diagnosed with pancreatic cancer within three years of the date of their diabetes diagnosis. The high-risk screening clinic will be expanding to screen new-onset diabetic patients during this three-year window.
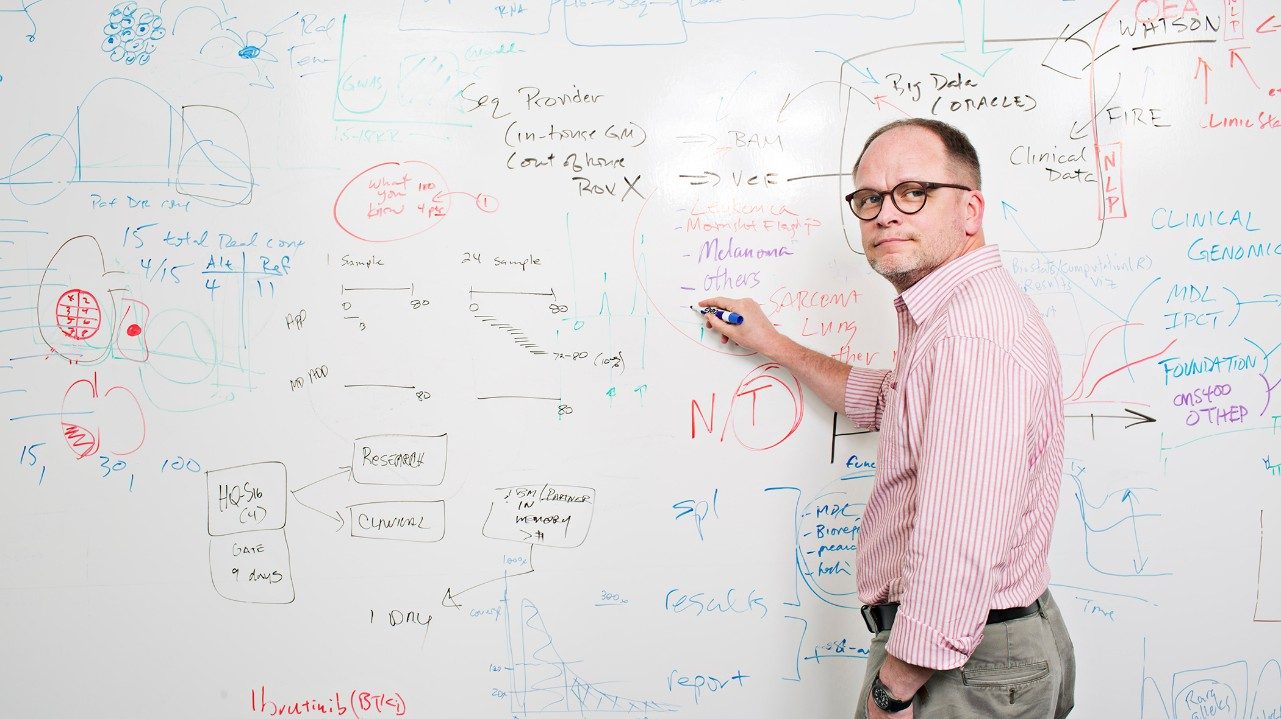
Novel screening tests
To date, no screening test has been conclusively shown to lower the risk of dying from pancreatic cancer, and only about 6% of patients are alive five years after diagnosis.
Funded by the Pancreatic Cancer Moon Shot, researchers are working to change that by creating a blood test that signals the presence of cancer. When developed, the test will detect cells that are shed from tumors or other substances that are produced in response to tumors.
They’re also investigating new imaging techniques to detect precancerous pancreatic lesions called PanINs (pancreatic intraepithelial neoplasias), early precursors of pancreatic cancer.
“They are unlike precancerous lesions for melanoma or polyps for colon cancer, which can be easily observed,” McAllister notes. “PanINs are microscopic lesions that can’t be seen by MRI.”