An immunotherapy drug to bolster a T cell surge
MD Anderson Melanoma Moon Shot researchers are combining two immunotherapies for the first time to double-team melanoma that has spread to other organs and resisted all forms of treatment.

Patients in a first-of-its-kind clinical trial will receive a vastly expanded dose of their own T cells — white blood cells that are the specialized warriors of the immune system — followed by a cancer immunotherapy drug known to promote the activation and survival of T cells.
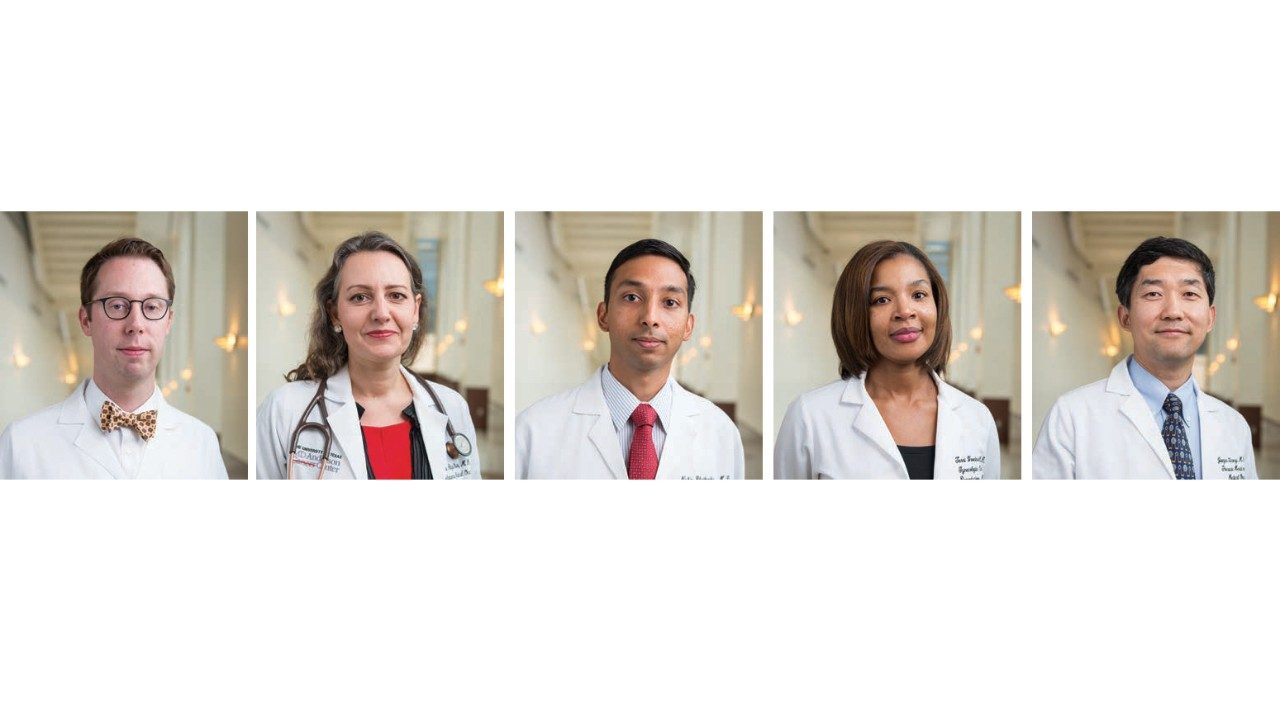
“We’re excited about this combination because there’s no standard of care now for our metastatic melanoma patients if immune checkpoint blockade drugs fail,” says clinical trial leader Rodabe Amaria, M.D., assistant professor of Melanoma Medical Oncology.
Checkpoint blockade drugs allow the immune system to unleash T cells to attack tumors. The drugs work by blocking molecules on T cells that act as brakes, which prevent the immune system from launching an attack. To date, researchers have developed two types of drugs that target two separate brakes. Brake No. 1 is called CTLA-4 and brake No. 2 is named PD1. The drugs have revolutionized melanoma treatment, producing powerful and lasting responses in about 10% to 30% of patients who take one drug only, and in more than 50% of those who take both drugs combined.
That still leaves substantial numbers of patients in need of a new approach. For checkpoint blockade to work, there have to be T cells primed and willing to attack the cancer.
Enter T cell expansion and infusion. T cells that attempt to kill cancer are often found in tumors that are removed or biopsied. There just aren’t enough of them to succeed.
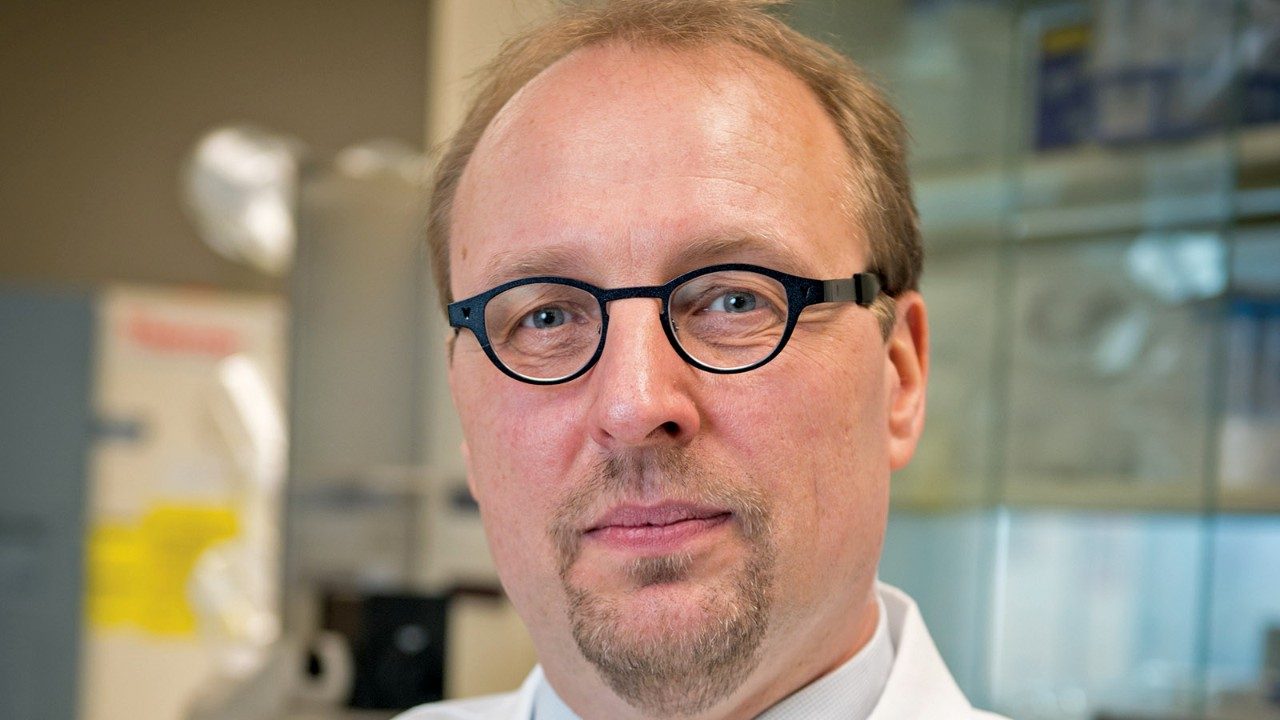
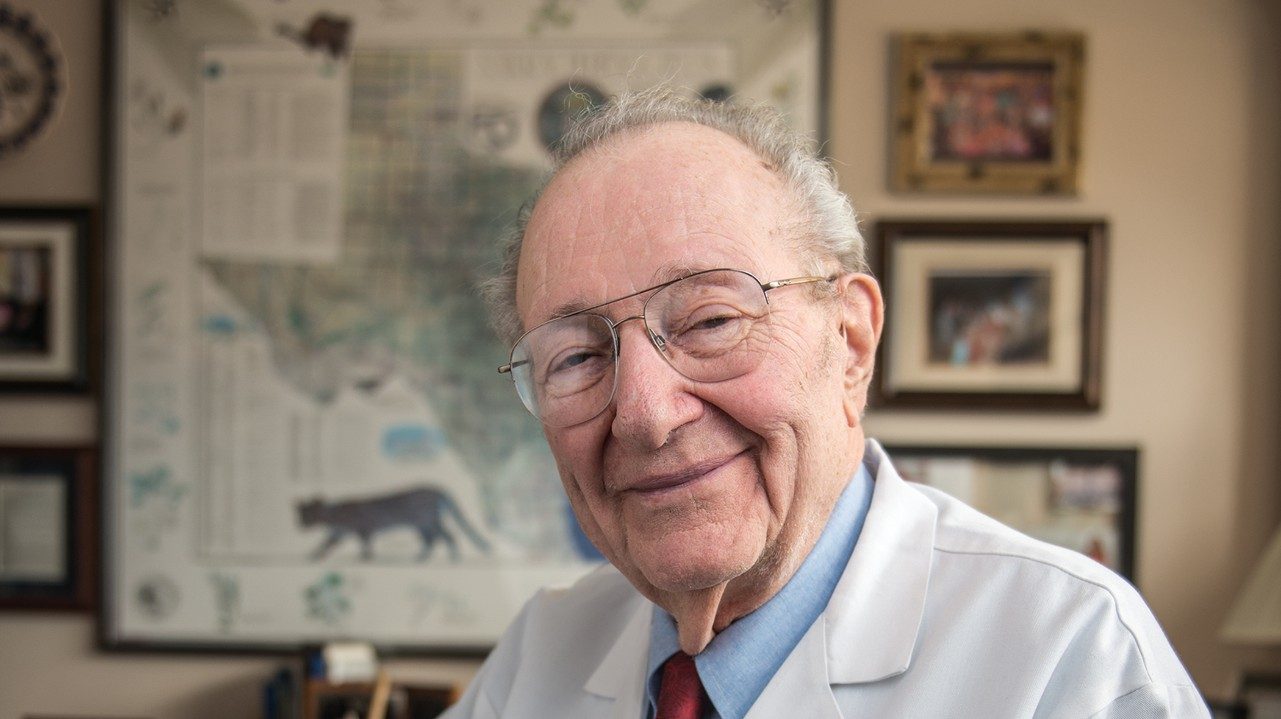
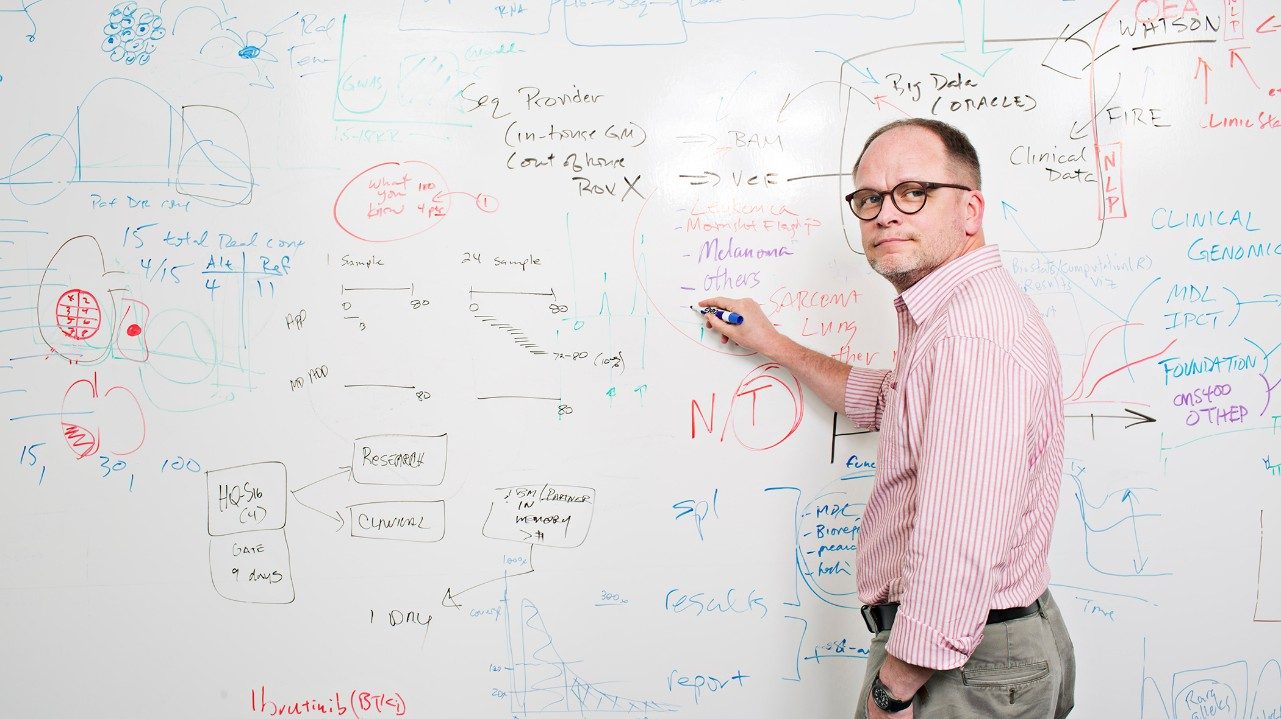
Patrick Hwu, M.D., head of Cancer Medicine and chair of Melanoma Medical Oncology, pioneered an approach that grows T cells on slices of a patient’s tumor in the lab, expands them to billions of cells over a few weeks, then infuses them back into the patient. The cells are called tumor-infiltrating lymphocytes, or TILs.
“We’ve treated about 100 patients with TILs. About 45 percent respond, and some of those responses last for years,” Amaria says. “There’s a lot of room for improvement.”
Patients in Amaria’s trial receive T cell expansion followed by a checkpoint blockade drug that blocks PD1. The trial is the first to combine TILs with a PD1 inhibitor.
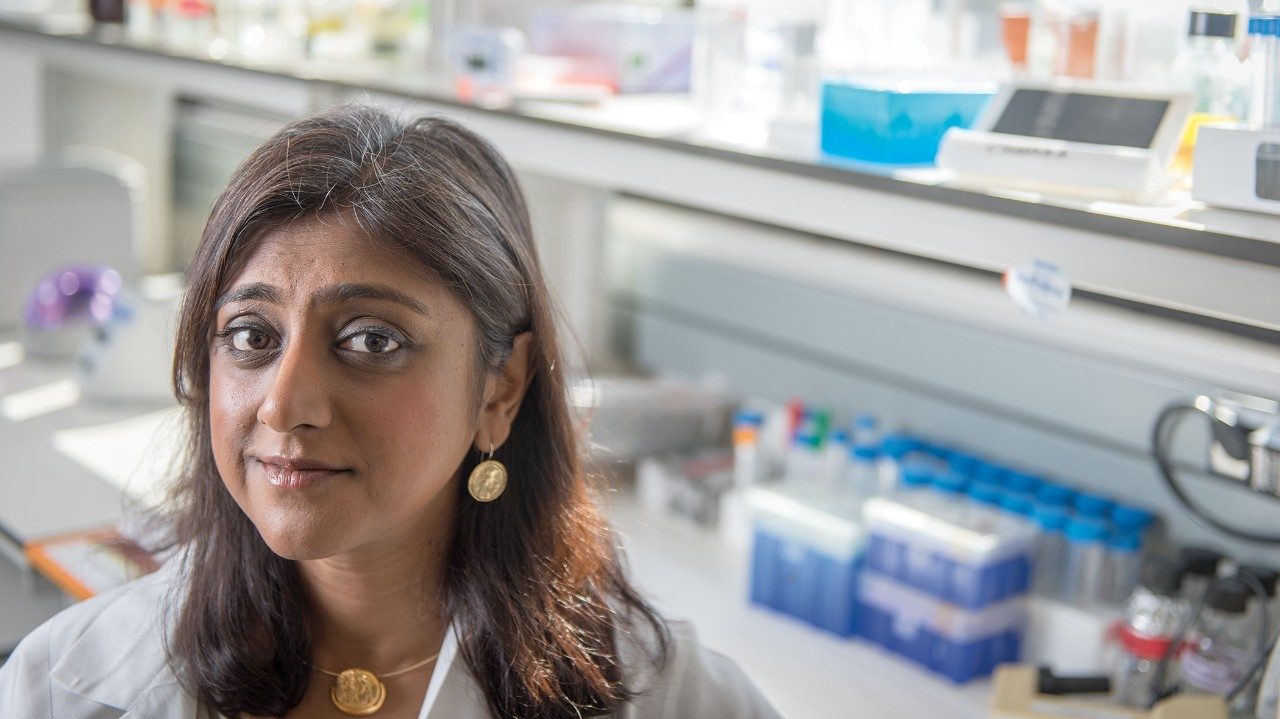
This double-whammy combination may also stimulate small proteins that fire up the immune system, according to research conducted in Hwu’s lab by Weiyi Peng, M.D., Ph.D. In the clinical trial, 36 patients with metastatic melanoma will have surgery, so their tumor-attacking T cells can be expanded and then frozen. They’ll then be hospitalized and treated with chemotherapy to reduce their existing T cells before being infused with their TILs.
After that, they’ll receive interleukin-2, an immune stimulating protein, to bolster immune response. Three weeks later, they’ll receive the PD1 inhibitor drug Keytruda.
Patients’ tumors are biopsied once before and at least twice after treatment.
“Biopsies are a priceless learning opportunity,” Amaria says. “It’s so important to see what’s happening in tumors throughout the course of treatment so we can understand and improve how we manage disease.”