Let’s protect ourselves against HPV-related cancers with the ‘cancer vaccine’

Kathleen Schmeler, M.D., vividly remembers the day a chance encounter on a flight to Amsterdam changed her life.
“The man sitting next to me happened to be reading the same novel I was, so we struck up a conversation,” says Schmeler, who at the time was a mechanical engineer with Procter & Gamble. “As it turned out, he was a colon cancer researcher and doctor in the Netherlands.”
Schmeler, who had always harbored an interest in medicine, chatted with her seatmate for six hours. The conversation led to a job offer.
“When we landed,” she says, “I called my parents to let them know I was quitting my job and moving to Amsterdam to work for a scientist doing cancer research.”
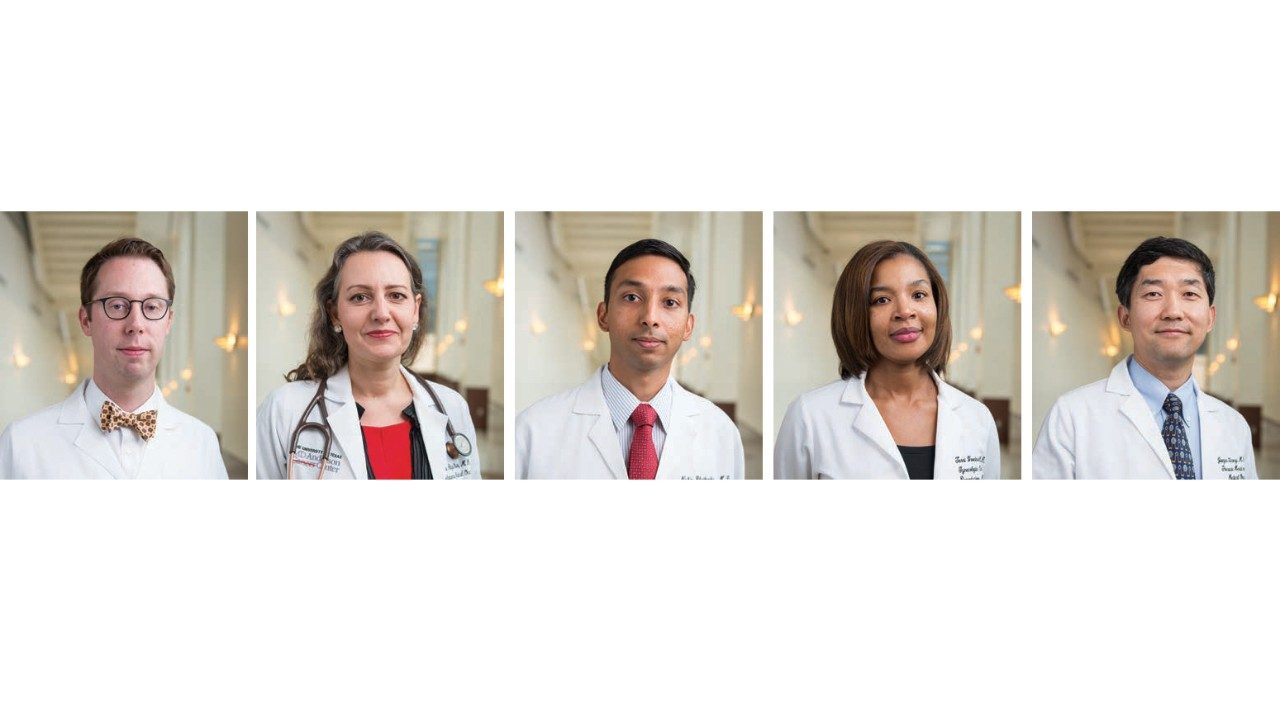
Twenty years later, Schmeler is an associate professor of Gynecologic Oncology and Reproductive Medicine and an impassioned advocate for women’s health. She’s on a mission to educate women — and men — about a vaccine that blocks transmission of the human papillomavirus (HPV), which causes 99% of cervical cancer. The virus also is linked to cancers affecting the middle throat and genital areas.
The HPV vaccine was approved by the Food and Drug Administration in 2006, and has the power to prevent all of these.
To the disappointment of Schmeler and others in health care, it’s been slow to gain wide acceptance.
“It’s disheartening,” Schmeler says. “We have to do a better job of getting it out there. It’s been slow, but we’re making strides.”
The Cancer Prevention Research Institute of Texas (CPRIT) awarded MD Anderson a $1.4 million grant to increase cervical cancer screenings and preventive treatments for underserved women along the Texas-Mexico border. CPRIT provides state funding for cancer research, prevention and product development programs. MD Anderson’s efforts target Cameron, Hidalgo, Willacy, and Starr counties, where the cervical cancer rate is 30% higher than anywhere else in the state, and 70% of the population is uninsured.
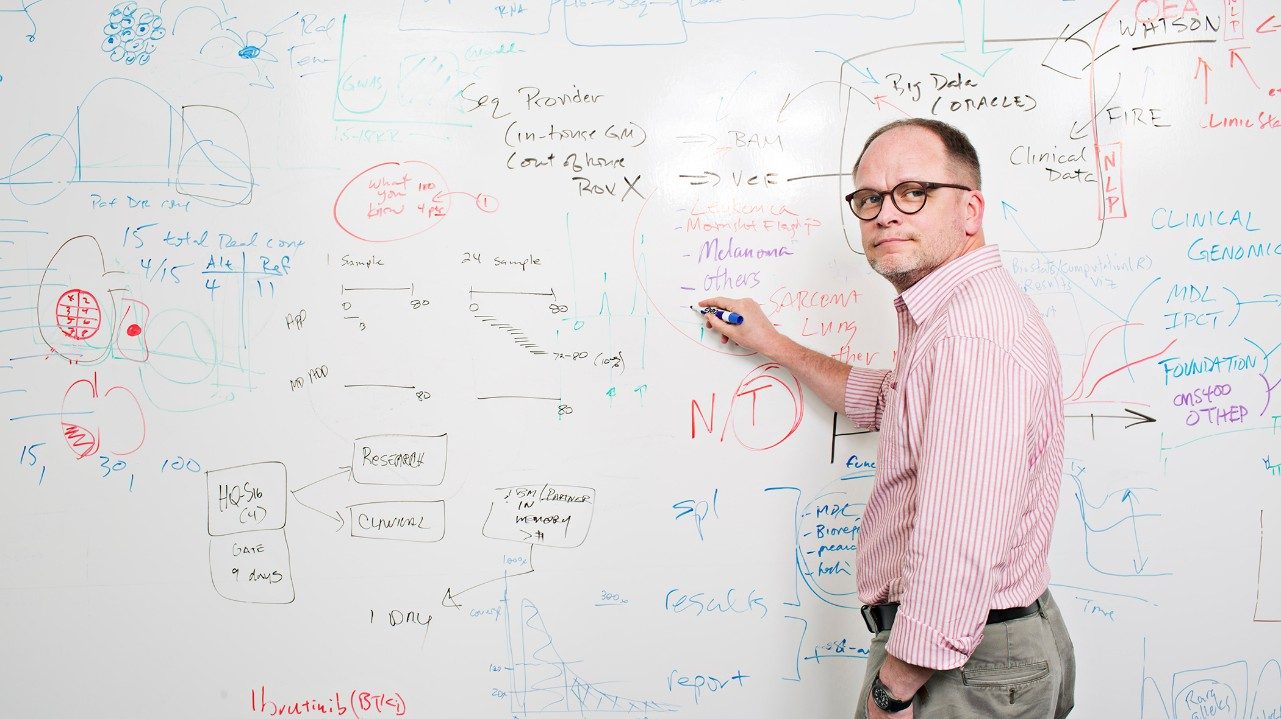
Last year, MD Anderson expanded its ambitious Moon Shots Program to include HPV-related cancers. Co-led by Schmeler, the moon shot’s goals include improving access and vaccination rates, developing HPV-related cancer screenings for men, developing targeted drugs that attack HPV-related cancers directly, and developing immunotherapies that rally the immune system to fight the virus.
“The moon shot has spurred us to organize our efforts and move our work benefiting patients to the next level. It’s not acceptable to make small, incremental improvements,” Schmeler says. “We must do something big and innovative on their behalf.”
Cervical cancer is the 14th most common cancer in the United States. Yet in Latin America, Africa and the Caribbean, it’s one of the leading causes of cancer deaths in women.
To bridge this gap, Schmeler and colleagues run the Central America Oncology Education Program, or CONEP. The program brings gynecologists from MD Anderson and other institutions to Guatemala, Honduras, El Salvador, Costa Rica and Panama, where they make patient rounds and train local doctors. Since CONEP’s inception in 2009, more than 100 Central American medical residents and faculty have participated in each of the visits. The program recently expanded to Mozambique in Southeast Africa.