Breast cancer screening guidelines aren’t a one-size-fits-all solution
It’s clear that breast cancer screenings save lives. But exactly when women at average risk of developing breast cancer should begin screening is much less clear.

Leading medical groups have conflicting guidelines. The American College of Obstetricians and Gynecologists (ACOG) and the National Comprehensive Cancer Network (NCCN) say starting at 40 is best. The U.S. Preventive Services Task Force (USPSTF) says women can wait until 50. And in October, the American Cancer Society (ACS) added to the confusion by revising its guidelines. For years, the ACS recommended women start mammograms at age 40, but the ACS now recommends starting at age 45, or at 40 if the patient chooses. The groups also vary on how often mammograms should be done. ACOG says annually, USPSTF says every two years, and the most recent ACS guidelines suggest getting annual mammograms between ages 45 and 54; after that, they say every two years is OK.
“My concern is that there is a lack of clear direction for woman and their doctors to best protect their health,” says Therese Bevers, M.D., medical director of MD Anderson’s Cancer Prevention Center.
To clarify the issue, Bevers urges a closer look at the new ACS guidelines. Although they recommend annual mammograms starting at 45, the guidelines suggest women should still have the opportunity to begin at 40.
“The guidelines still affirm the importance of annual screening for women in their forties and continuing for as long as they are in relatively good health,” says Bevers.
Additionally, the ACS now recommends against clinical breast exams for women. Given a lack of new data supporting this change, Bevers feels it’s premature to recommend against this important clinical practice.
“Annual clinical breast exams are a chance for women to meet with their doctors to discuss screening, risk and healthy lifestyles to reduce their breast cancer risk.”
In line with the ACOG and the NCCN guidelines, MD Anderson continues to recommend annual screening and clinical breast exams beginning at 40.
“Our mission is to save lives, and data has shown this approach to be the best way to do that,” says Bevers.
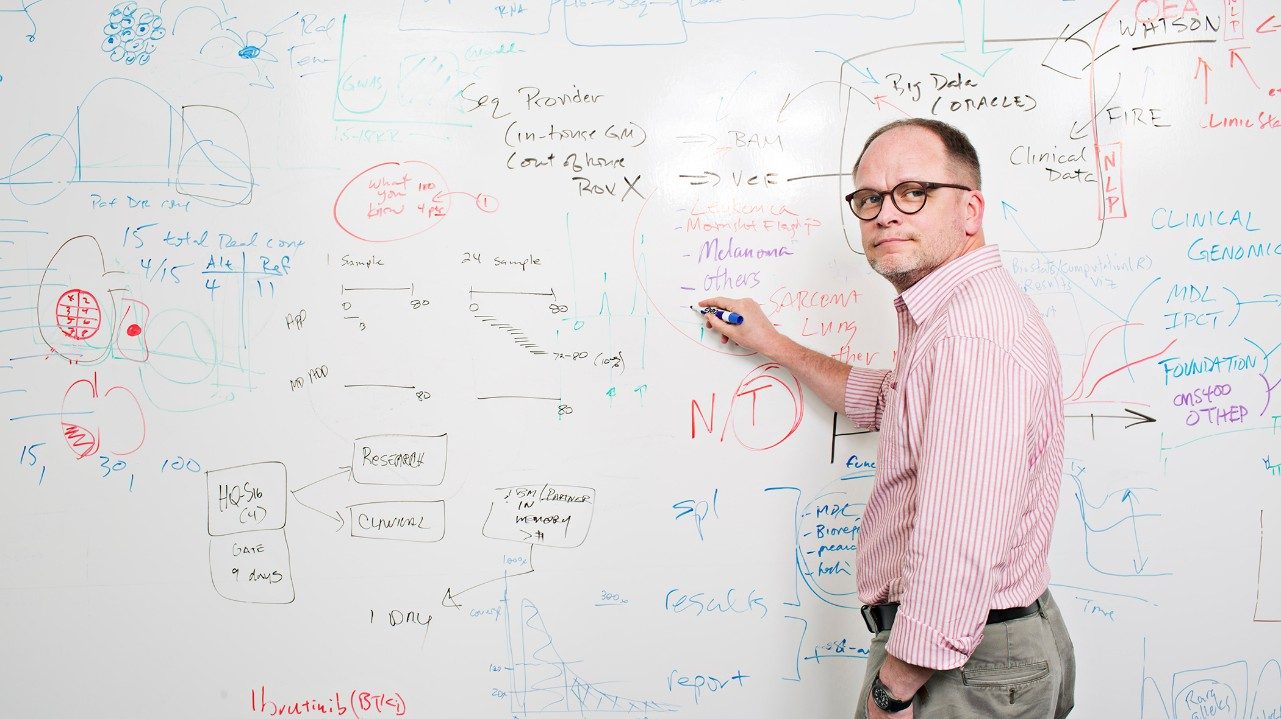
Screening for women at elevated risk
The above recommendations, however, apply only to women at average risk of breast cancer — not to those at elevated risk.
“There are many factors that may increase a woman’s risk, including family history, hereditary cancer syndromes, previous cancers, age when first giving birth and age at first menstrual cycle,” says Jennifer Litton, M.D., associate professor of Breast Medical Oncology.
Unfortunately, for those at high risk, there’s no single answer for screening.
“Screening recommendations for women at increased risk depends on why they are at increased risk,” explains Litton.
Depending on the situation, it may be appropriate to get screened earlier, more often or in different ways.Women should talk to their doctor to determine their risk, as well as individualized recommendations for screening or risk reduction. Risk assessment tools also are available from MD Anderson and the ACS.

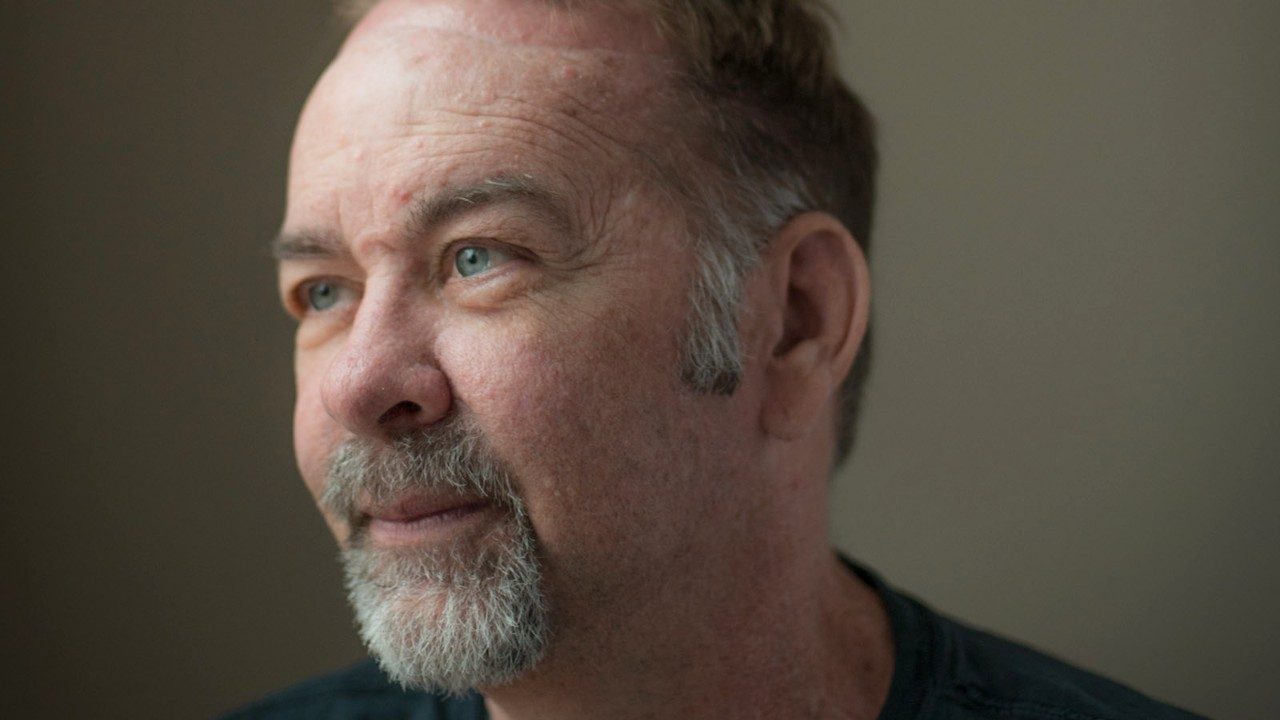
Michelle Baumann
Baumann asked to get her first mammogram before she was 40 because her grandmother had breast cancer. As the mother of two young boys, she wanted to start her annual screenings early.
Her doctor agreed and nine months before her 40th birthday she was diagnosed with Stage 1 breast cancer. Because her cancer was caught early, Baumann’s treatment consisted of a bilateral mastectomy and reconstruction.
“The thought of waiting until 45 for screening is scary,” says the elementary school principal. “I would’ve been six years into my cancer by that point. You have to trust your gut, advocate for yourself and become a part of the process.”

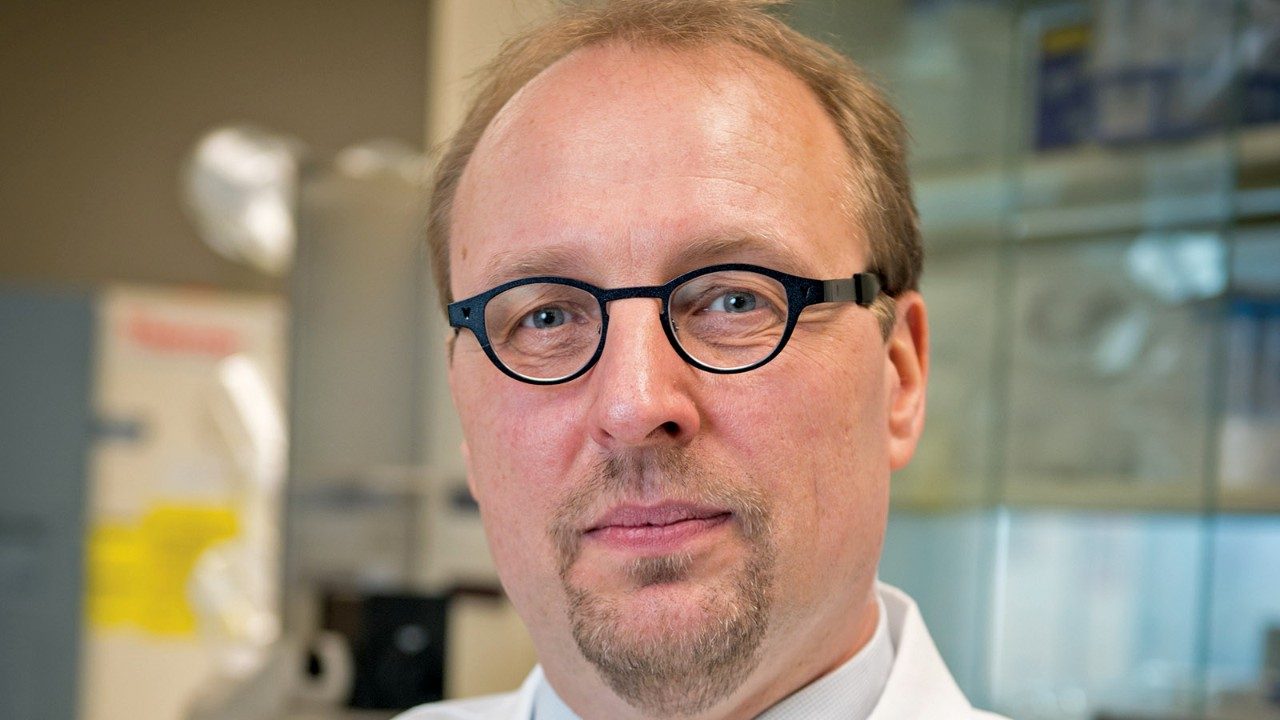
Nancy Lombard
Lombard is an advocate for early detection. She began having her annual mammograms at age 40. Three decades later, when she was 70, she decided to have a 3D mammogram for the first time. With this technology, doctors caught a Stage 1 cancer in her left breast, one that a standard mammogram would have missed.
Following her surgery, a CT scan revealed a small tumor in her lung that required a lobectomy. By catching both cancers early, Lombard successfully overcame breast and lung cancer in just a year.
With no family history of cancer she could have elected less-frequent screening, but she believes it’s important to be vigilant. Lombard says she’ll be sure to emphasize the importance of yearly mammograms to her two daughters and four granddaughters.
“I think screening is very important,” she says. “Based on my experience, why take the chance? If these cancers hadn’t been caught early, they would probably have already spread to other parts of my body.”

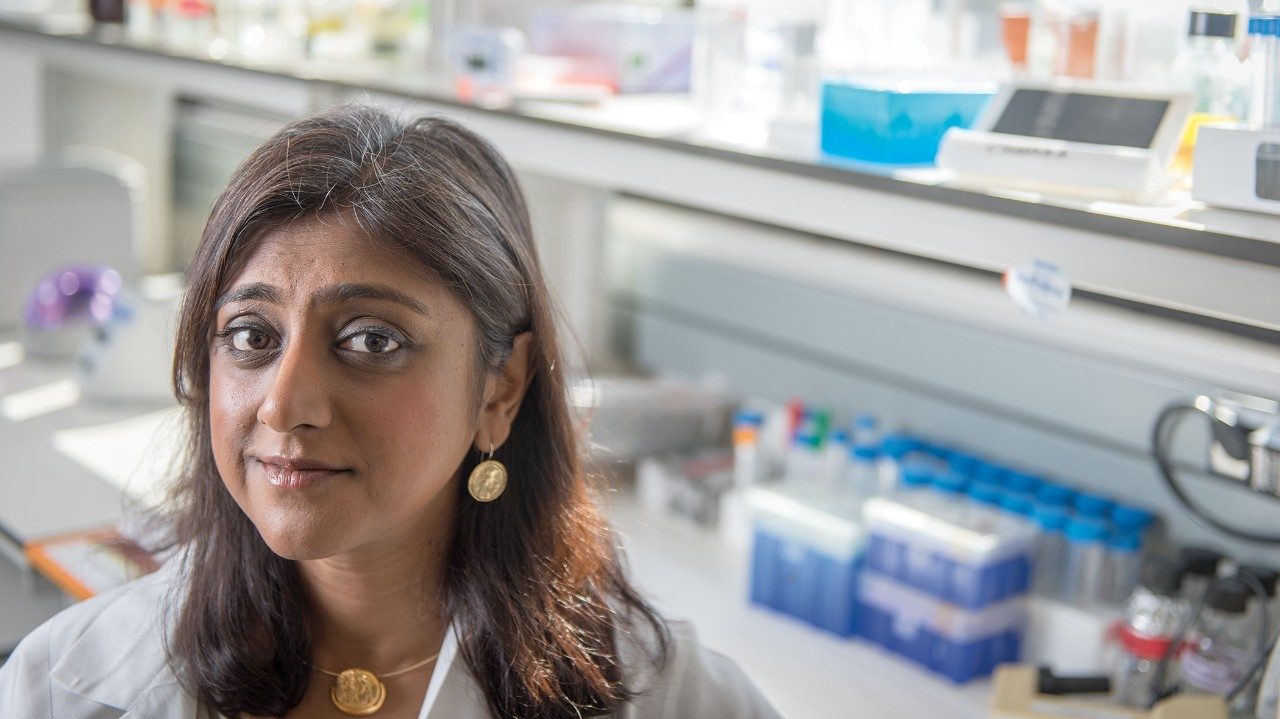
Roxana Lopez
Lopez, an aspiring nurse, was diagnosed with Stage 2 breast cancer during a clinical breast exam when she was 25, two decades younger than the ACS’ recommended screening start date for women at average risk of cancer. But Lopez wasn’t average. After genetic testing confirmed she carried a BRCA1 mutation, she urged her twin sister, Ana, and two brothers to get tested. Turns out all three also have the mutation that increases the risk of breast and ovarian cancers in women. That wasn’t entirely a surprise; their mother was diagnosed with breast cancer at 47, and died four years later.
After completing chemotherapy, Lopez will undergo a double mastectomy to reduce the risk of recurrence. Her sister is also having a preventive double mastectomy to reduce her risk of developing breast cancer.
“I still have a goal of going to nursing school. I look forward to getting all my treatments done and getting better, and then being able to move on with my life.”