The Nocturnal Program: Care, uninterrupted
The Nocturnal Program ensures a seamless transition from day to night for patients

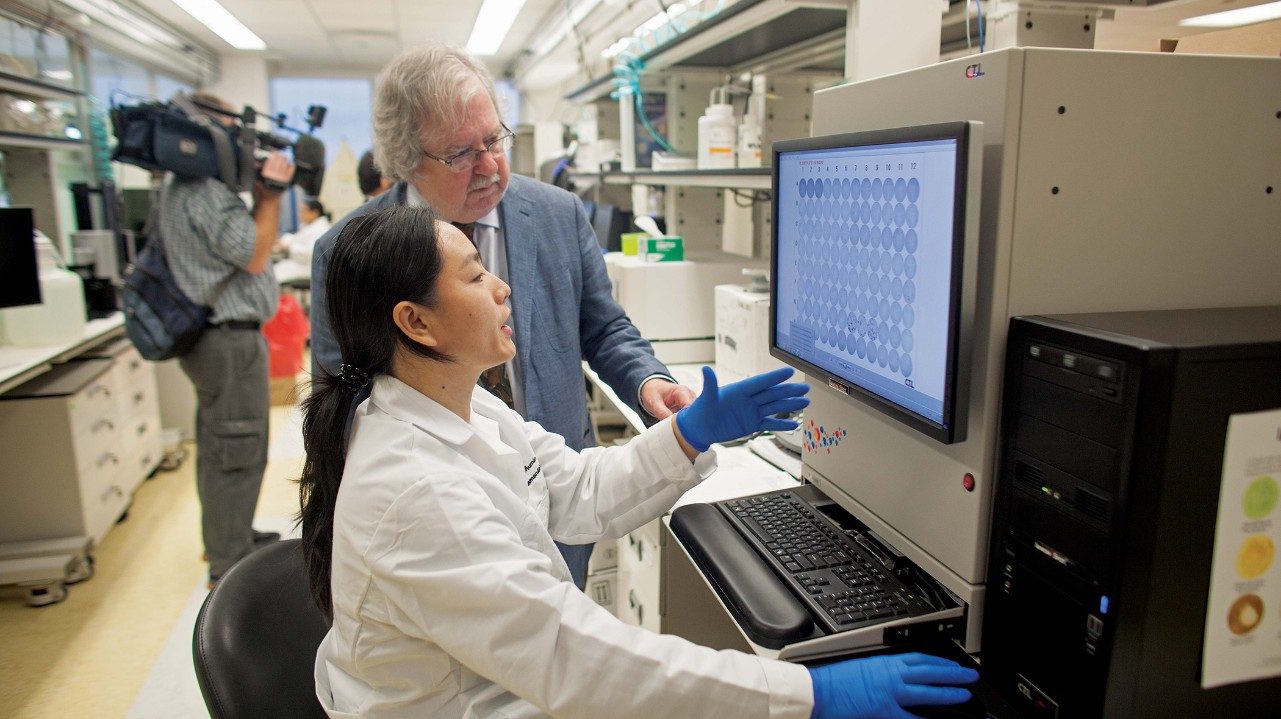
In the still of the night, MD Anderson traffic slows, hallways hush and quiet sets in. But when it comes to the critical needs of patients in the hospital, there’s no downtime.
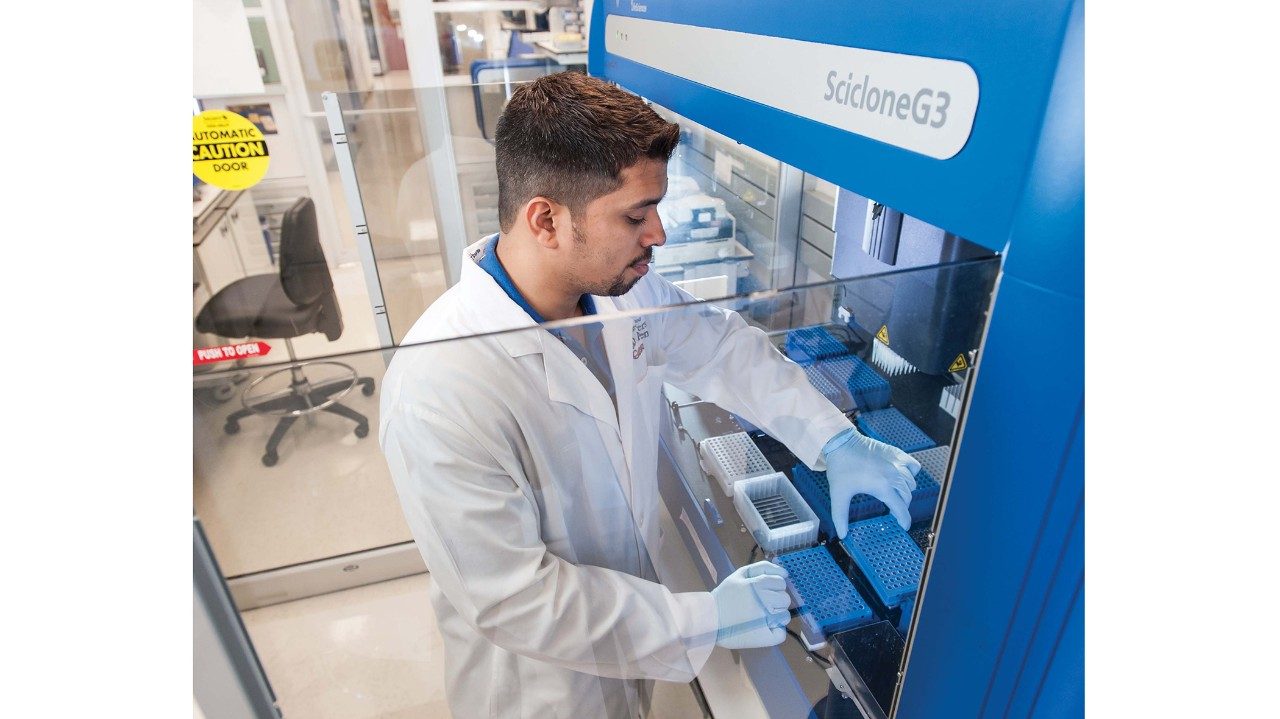
MD Anderson’s Nocturnal Program provides an extra layer of care. The teams of six physicians, two trainees and nine midlevel providers complement the overnight nursing teams on each unit and respond to a wide range of calls from colleagues on inpatient floors, the Intensive Care Units and the Children’s Cancer Hospital.
They see adult and pediatric patients contending with their individual cancer battles: spiked fevers, fluctuating blood pressures and electrolyte imbalances. The team also is called to units to update patients’ families with the latest information on loved ones, clarify orders written by the dayshift or check out an attentive nurse’s hunch that something isn't right.
Launched two years ago, the program expanded its reach in 2013 to include pediatric and surgical services, as well as the size of its staff. The ratio of patients to physicians during the overnight hours now is 50 to 1. The national average for an overnight program is 60-70 to 1.
The Nocturnal Program
Ratio of patients to physicians: 50:1
Number of providers: 150
24/7 quality: “We make sure the same quality of care is delivered to our patients at night as during the day.”
“The Nocturnal Program has reduced the number of night calls to physicians at home by at least half, possibly more.”

While you were sleeping
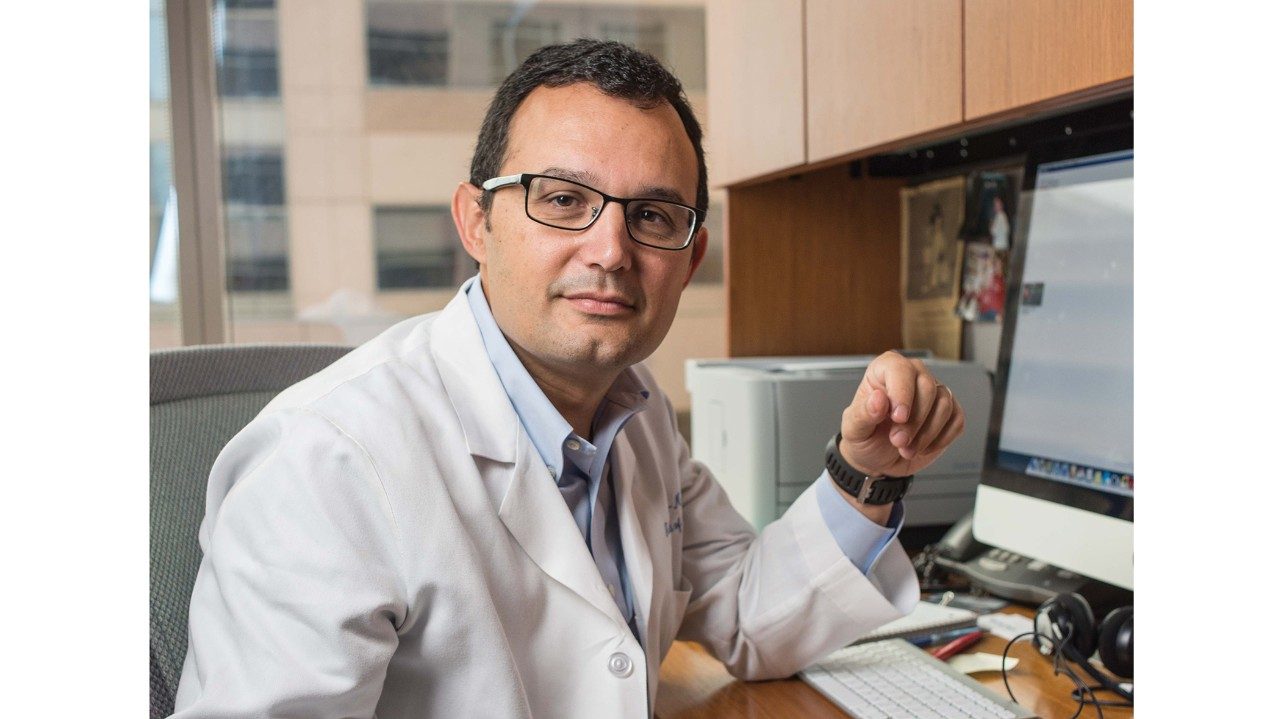
Karen Chen, M.D., spends the majority of her time in the busy Intensive Care Unit treating patients who are among the sickest at MD Anderson.
Working nights as medical director for the Nocturnal Program, Chen, professor in Critical Care, may be anywhere in the 600-bed Alkek Hospital caring for a variety of patients with a range of symptoms or conditions.
She may be found consulting with an attending physician by telephone, discussing a change in a patient’s condition. She may be seen talking to a family member who just got off work and is eager for an update on a loved one. Or she may be comparing notes with a trainee about his or her assessment of a patient.
Her role carries as many responsibilities as there are phases of the moon.
“We make sure the same quality of care is delivered to our patients at night as during the day,” Chen says. “We’re focused on individual episodes of care, taking care of patients who are sick or who could get sick very suddenly. So we must collaborate effectively with those team members who work during the day, including the attending physician or surgeon, who often is at home.”
Chen built the Nocturnal Program from the ground up, starting with 90 MD Anderson physicians and fellows, moonlighting physicians from around the Texas Medical Center and trainees. She later added a cadre of midlevel providers. Now with a pool of more than 150 providers available for overnights, they’re scheduled well in advance of their shifts and day jobs so there’s ample time for rest. Plus there are on-call rooms with sleeping quarters.
“We want our colleagues who work during the day to be very comfortable with the care we provide when they’re not here, and that means close collaboration and solid medical decisions,” Chen says. “We work toward that goal every night.”