Nowhere to hide
By exposing cancer cells, fluorescence makes surgeons’ jobs easier.

It’s easy to see, pardon the pun, why urologists and gynecologic surgeons would be excited by the promise of medical fluorescence.
With it, surgeons can light up hard-to-see cancer cells during minimally invasive surgery.
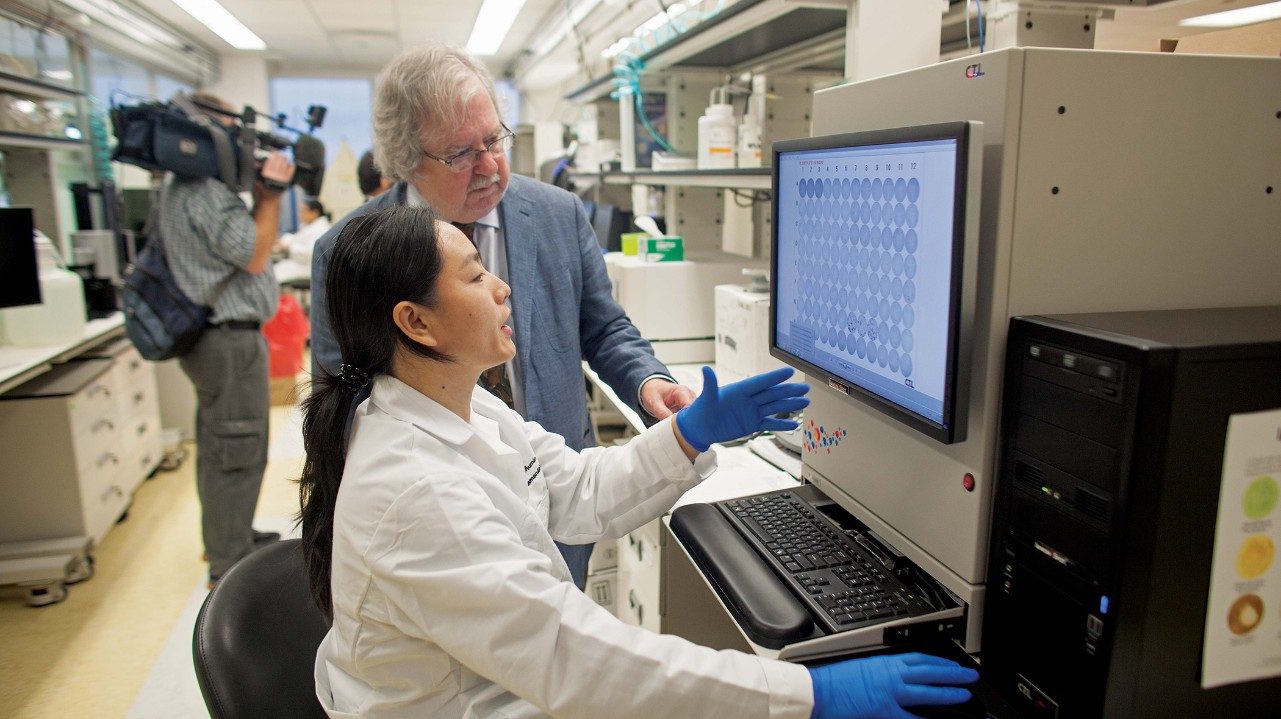
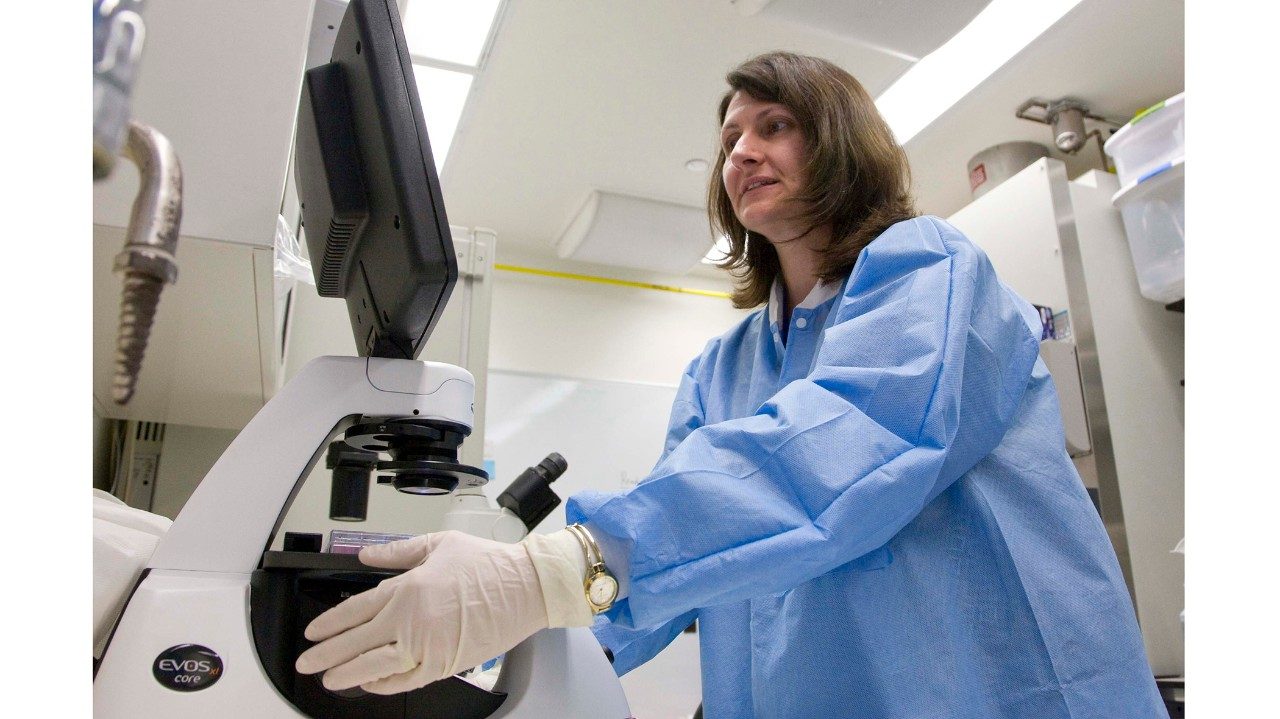
“It illuminates the target, not the entire surgical field, when you activate the fluorescent light,” explains Nicole Fleming, M.D., assistant professor in Gynecologic Oncology and Reproductive Medicine at MD Anderson’s regional care center in Sugar Land.
She uses indocyanine green (ICG) dye to help illuminate the patient’s blood supply and lymphatic system. Fleming is looking specifically for tumor perfusion and lymph nodes affected by cervical or endometrial cancer cells.
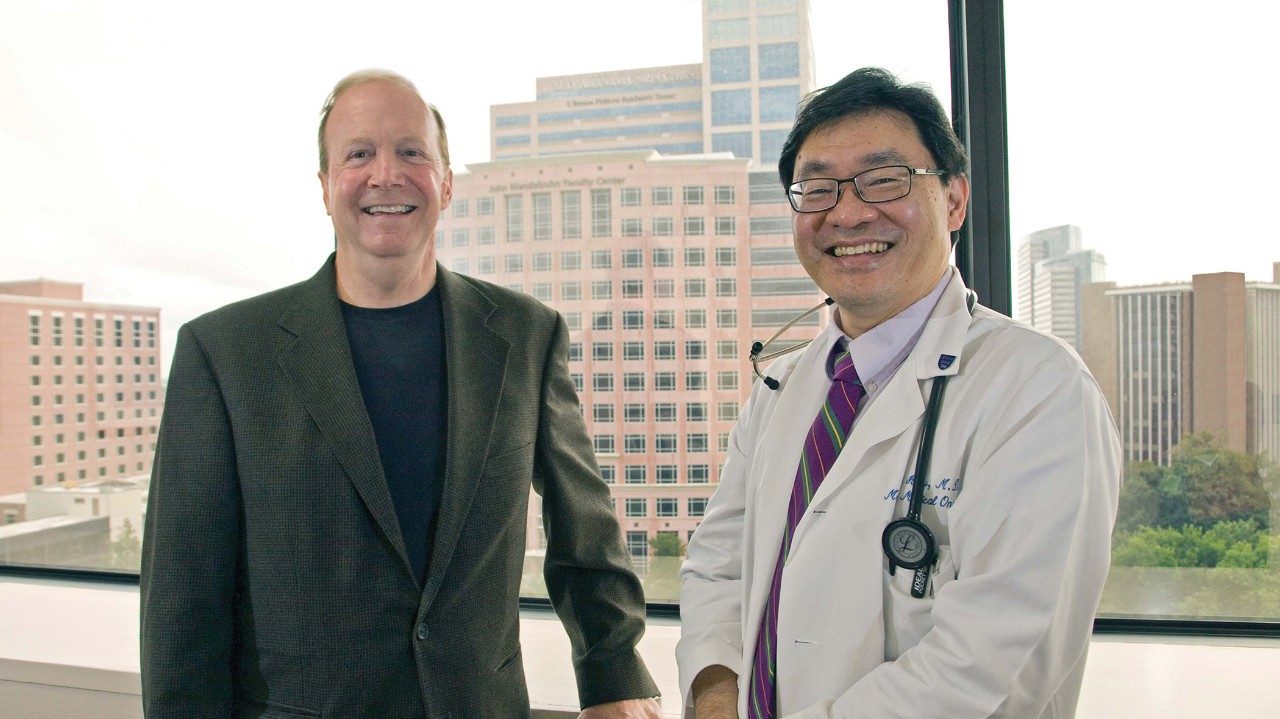
H. Barton Grossman, M.D., a clinical professor in Urology, injects hexaminolevulinate hydrochloride, a colorless solution, to turn bladder tumors pink under blue light.
“This technology highlights cancers that, under white light alone, look perfectly normal,” Grossman says.
He led a 2007 randomized study that followed more than 800 patients over nine months. Blue-light cystoscopy better distinguished carcinoma in situ (cancer that hasn’t metastasized), as well as the parameters of papillary tumors in study participants, making the tumors easier to find and remove.
Participants later showed improved time to recurrence (16.4 months) than those exposed only to traditional white-light cystoscopy (9.4 months).
While fluorescence is not appropriate for every surgical case, Grossman estimates it benefits one out of five bladder cancer patients in which it’s used.
Fleming, too, is excited by the potential for medical fluorescence. “I think this is just the start of where we’re going with this.”