Building a better T cell
Treatments relying on T cells, a key component of the body’s immune system, have had significant success, but a new experimental method customizes naturally produced cells to sharpen their attack on cancer.
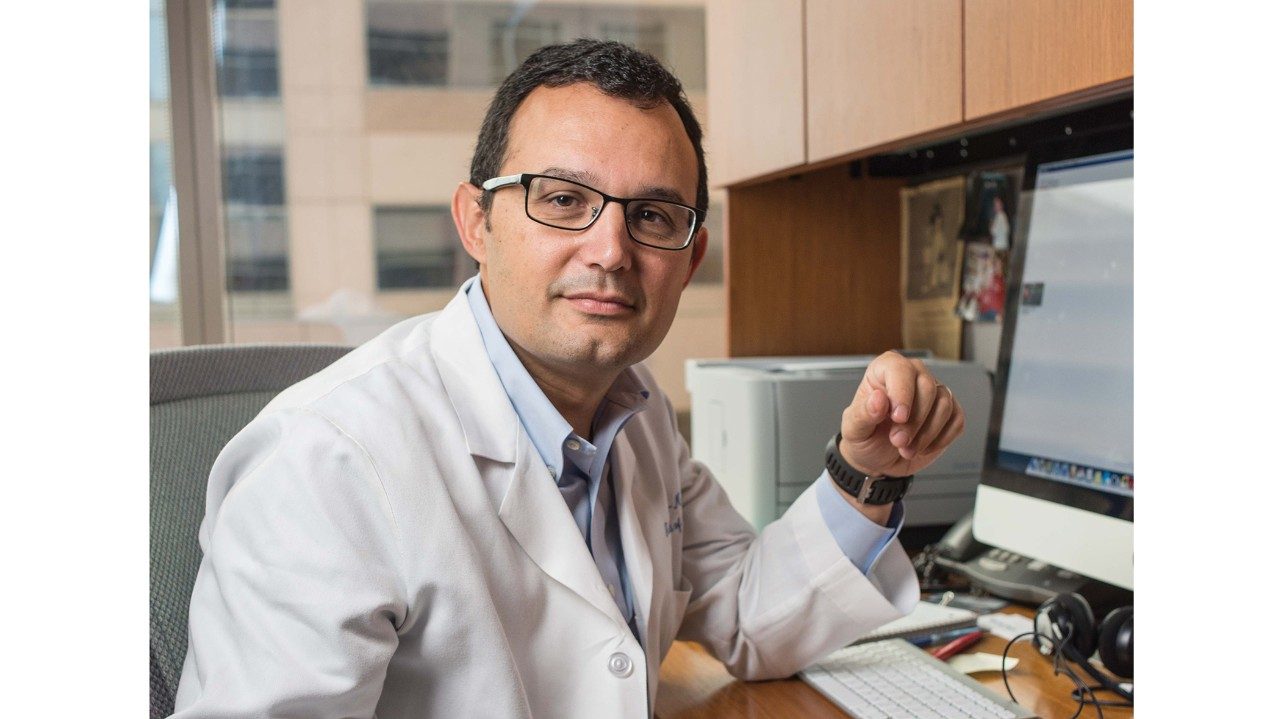
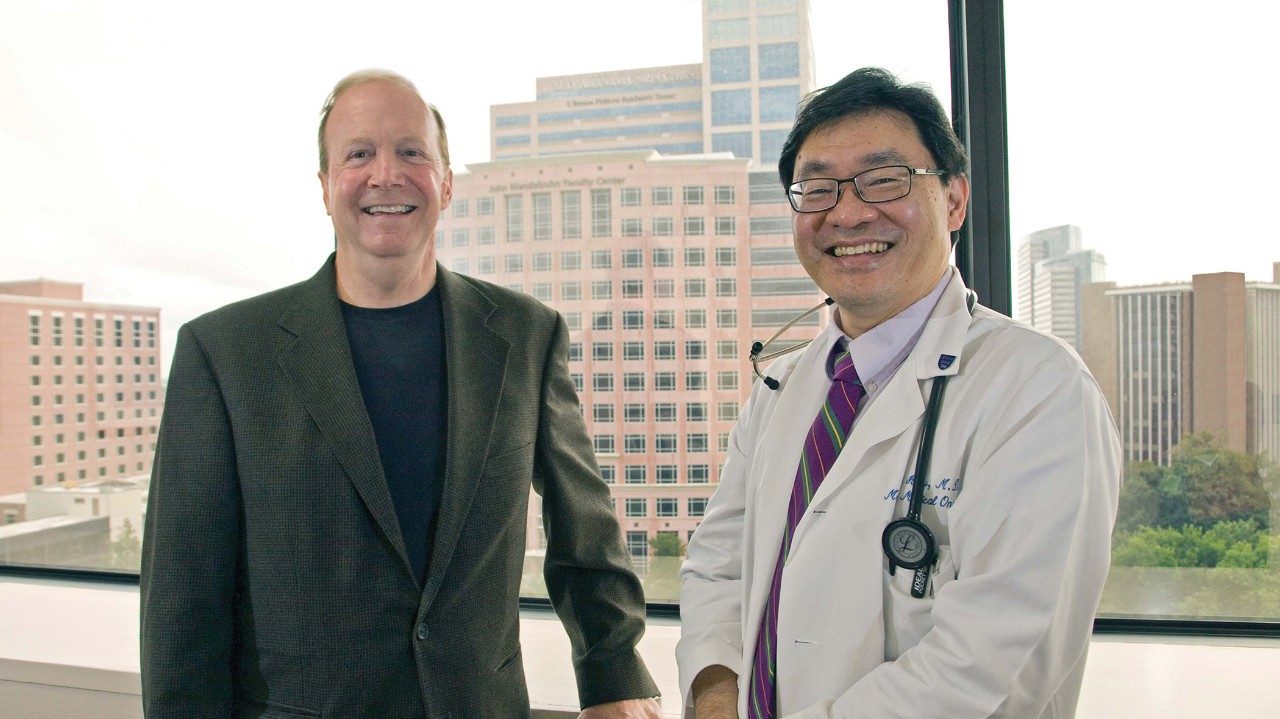
“Instead of relying on the body’s own ability to create the right T cell, we insert designer receptors generated in the lab to reprogram T cells and improve their ability to target tumors,” says Laurence Cooper, M.D., Ph.D., professor in Pediatrics.
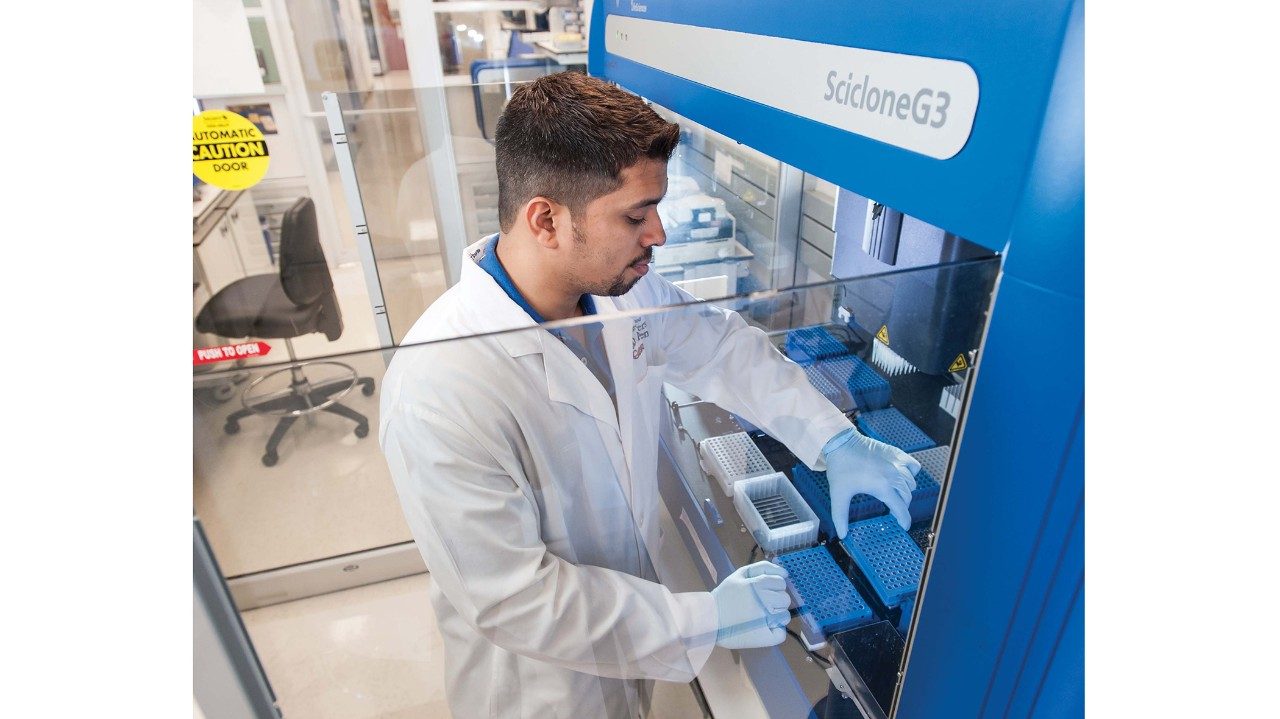
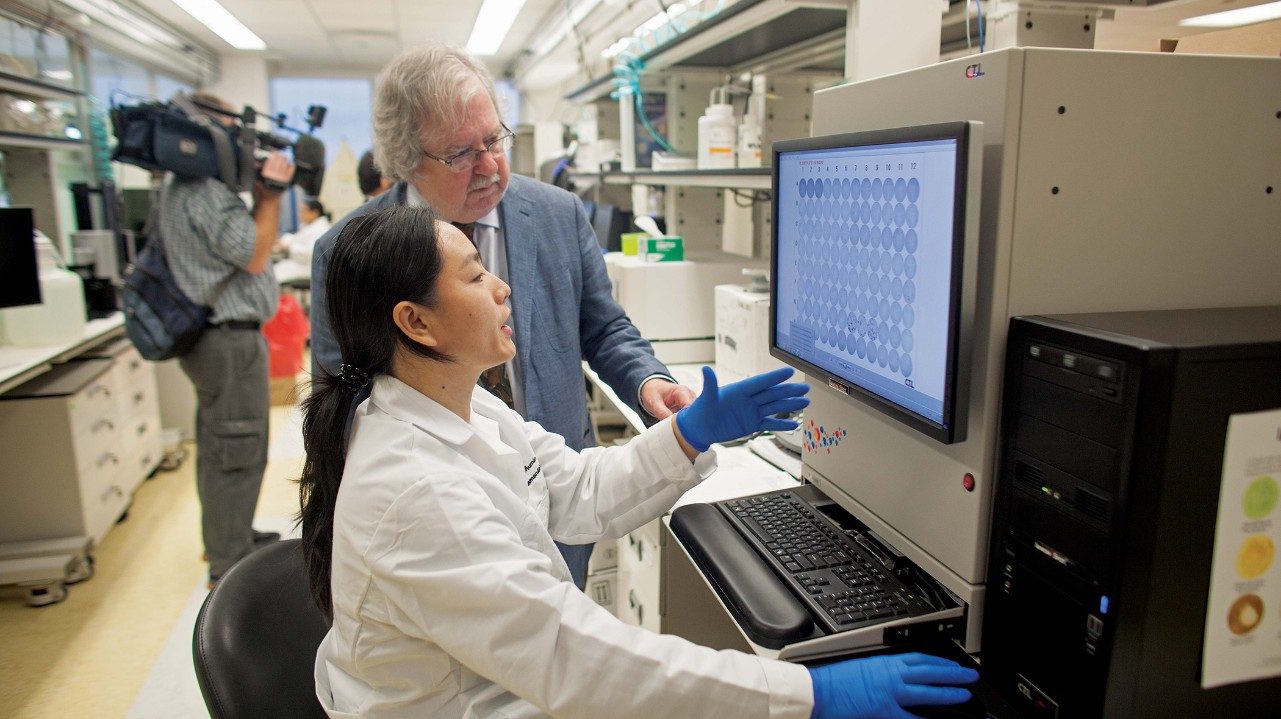
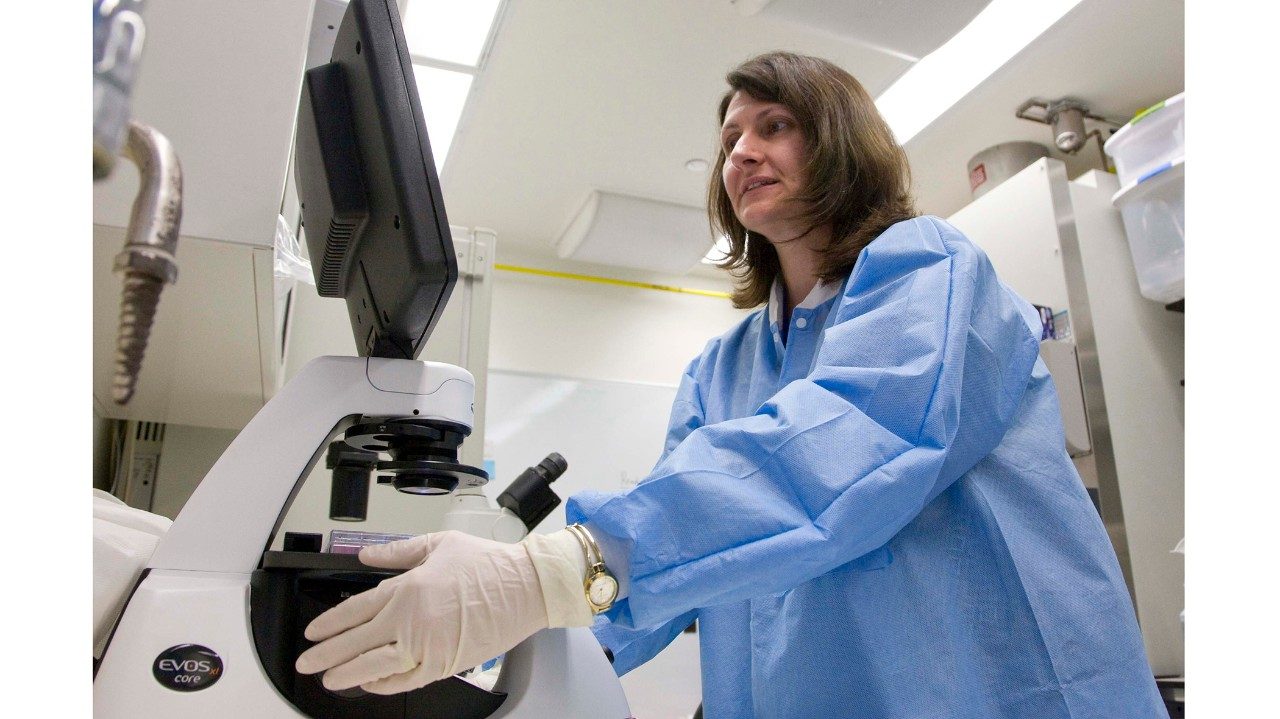
A team of scientists and clinicians developed the therapy, which now is employed in clinical trials for various blood cancers. A new gene transfer system initially developed by a scientist at the University of Minnesota to modify fish has been adapted by Cooper and his group to install genes that create a receptor on T cells. That receptor, called a chimeric antigen receptor (CAR), is a molecule on the surface of a cell that can bind with other cells. When the CAR docks with cancer cells, it triggers a T cell attack to kill tumor cells.
Early clinical trial results have been promising when these CAR-modified T cells are given to patients after they receive a blood stem cell transplant to treat their leukemia or lymphoma. The idea, Cooper says, is to provide an added boost to the anti-cancer response.
A clinical trial opened in late 2013 that provides CAR therapy immediately after chemotherapy for leukemia. These trials lay the foundation for targeting solid tumors such as pancreatic cancer.
For now, access to CAR T cells, which are made in a highly specialized lab environment, is limited — something Cooper hopes to change.
“Our vision is to streamline this process so that these cells can be broadly available at reduced cost,” he says.
The CAR key
What it is: Chimeric Antigen Receptor
How it works: The CAR allows a T cell to dock with cancer cells and triggers an attack.
The doctor says: “We insert designer receptors generated in the lab to reprogram T cells and improve their ability to target tumors.