- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (66)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (28)
- Bladder Cancer (68)
- Brain Metastases (28)
- Brain Tumor (230)
- Breast Cancer (716)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (154)
- Colon Cancer (164)
- Colorectal Cancer (110)
- Endocrine Tumor (4)
- Esophageal Cancer (42)
- Eye Cancer (36)
- Fallopian Tube Cancer (6)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (6)
- Kidney Cancer (124)
- Leukemia (344)
- Liver Cancer (50)
- Lung Cancer (288)
- Lymphoma (284)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (98)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (170)
- Pancreatic Cancer (166)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (144)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (236)
- Skin Cancer (294)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (60)
- Testicular Cancer (28)
- Throat Cancer (90)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (78)
- Vaginal Cancer (14)
- Vulvar Cancer (18)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (624)
- Complementary Integrative Medicine (24)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (230)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (122)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (892)
- Research (390)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (404)
- Survivorship (322)
- Symptoms (184)
- Treatment (1772)
Glioma vs. glioblastoma: What’s the difference?
BY Lauren Rose
4 minute read | Published February 18, 2022
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on February 18, 2022
Glioma and glioblastoma might sound similar, but there are differences between these two types of brain tumor diagnoses.
Here, neuro-oncologist Ashley Aaroe, M.D., explains the distinctions between glioma and glioblastoma – and shares insights on their diagnoses and treatments.
Glioblastoma is a type of glioma
A glioma is one of the most common categories of primary brain tumor. Glioblastoma is a type of glioma.
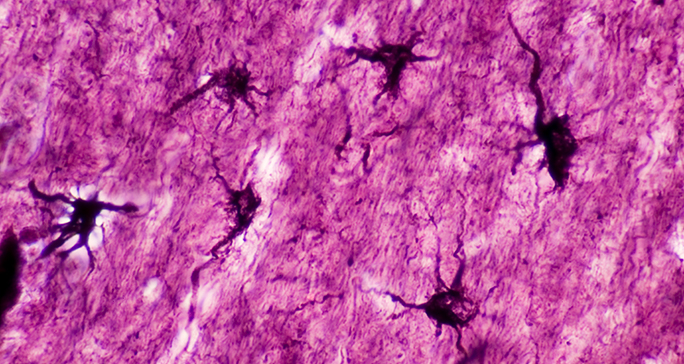
Glioma is an umbrella term for cancer of the glial cells that surround nerve endings in the brain. Glial means “glue,” and these cells provide support for neurons, which are responsible for walking, talking, thinking, seeing, and more.
“Think of it this way: neurons are like messy teenagers; they don’t clean up after themselves and need help from their parents,” Aaroe says. “They need glial cells to help protect them, clean up after them and help nourish them. When something goes wrong, glial cells turn into a glioma. In most patients, we don’t know what causes this.”
- Related: Glioblastoma symptoms
Gliomas are categorized by grade
Many gliomas are named for the type of glial cell they most closely resemble. Slower growing gliomas are also called “low grade.” These include Grades 1 and 2 gliomas. High grade gliomas are Grades 3 and 4. Gliomas are graded based on how aggressively or rapidly the cells divide. The higher the grade, the more aggressive the brain cancer is. By definition, a glioblastoma is always a Grade 4 glioma.
Low grade tumors are typically seen more commonly in younger patients. Older patients are more likely to have a higher grade diagnosis like glioblastoma. These are some of the most common types of gliomas categorized by grade:
- Grade 1: There are many kinds of Grade 1 gliomas. Pilocytic astrocytomas are one example. These are more common in children.
- Grade 2: Diffuse glioma, either astrocytoma or oligodendroglioma.
- Grade 3: Anaplastic glioma, either astrocytoma or oligodendroglioma.
- Grade 4: Either glioblastoma IDH wildtype or IDH-mutated astrocytoma. Glioblastoma IDH wildtype is the most aggressive.
How glioma and glioblastoma are diagnosed
Thanks to advances in diagnostic techniques, doctors are able to make more precise glioblastoma and other glioma diagnoses.
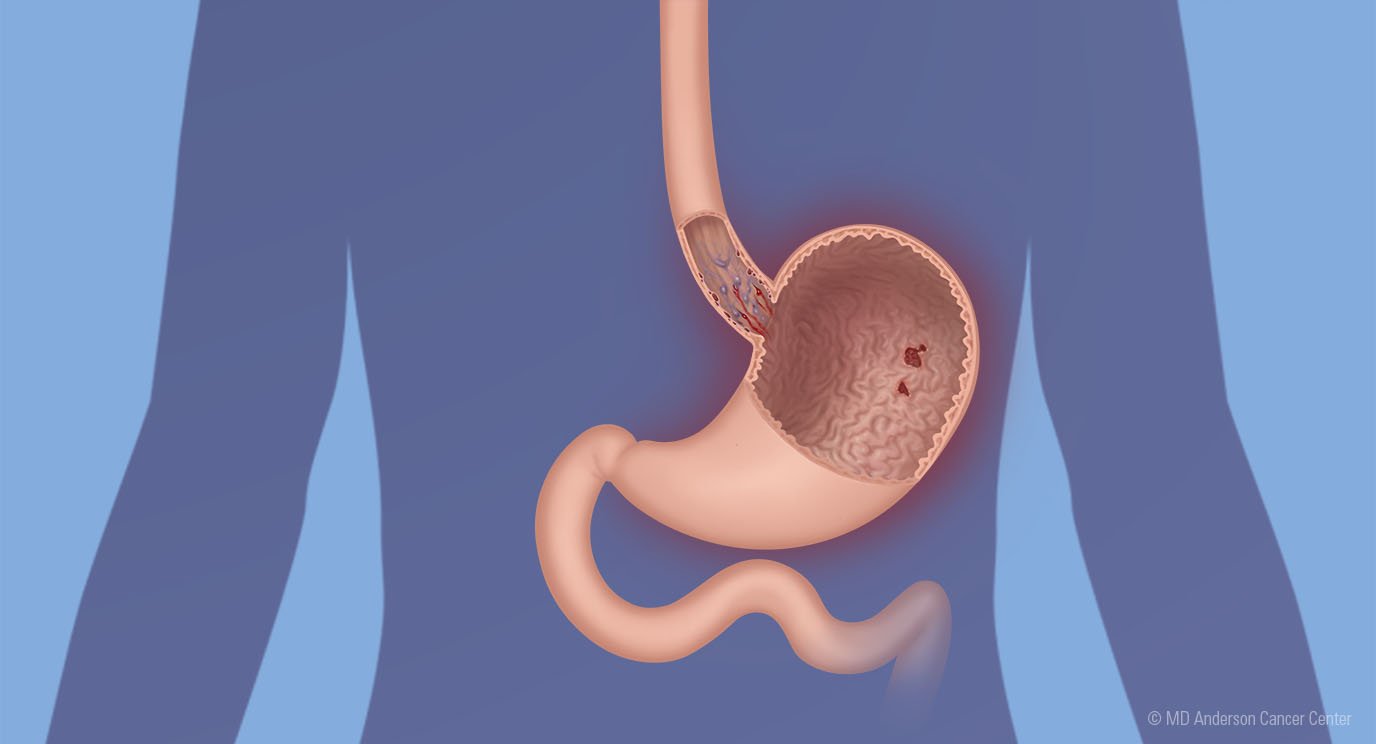
The most common imaging test for glioma is an MRI. If the MRI shows a tumor, your physician will most likely want to take a sample to perform a biopsy. A biopsy is a surgical procedure where a piece of the tumor is cut away and removed for testing. The sample will be sent to a laboratory for analysis. After the sample arrives in the lab, a pathologist will inspect the tissue. Doctors used to only look at cancer cells under a microscope to identify the glial cell. Now, they’re able to identify these types of tumors by their molecular features, which are the genetics within the cancer cells themselves.
In 2021, the World Health Organization (WHO) updated their classification of tumors of the central nervous system, which includes gliomas. A tumor’s cancer cells might look like a lower grade glioma under a microscope, but the genetic features of the tumor might show that it acts more like a glioblastoma. This means the tumor could be more aggressive than originally thought.
Certain genetic features can distinguish between different kinds of gliomas. Physicians test for IDH, an enzyme that affects metabolism in the cancer cells. Testing is also done for the genetic marker 1p19q, which helps distinguish oligodendroglioma and astrocytoma.
Risk factors for gliomas and glioblastoma
While gliomas usually occur at random, there are two known situations that might cause a glioma to form. If a person has had radiation therapy to treat head and neck or brain cancer at a young age, they are at a higher risk for secondary cancers. If genetic diseases run in a patient’s family, this might stem from a glioma diagnosis. Otherwise, there are no known factors that cause gliomas.
While there are no modifiable risk factors for glioblastomas, male patients who are in their 50s are more likely to be diagnosed with this kind of tumor.
Treatments for glioma and glioblastoma differ, too
Most of the time, gliomas tend to infiltrate the brain. When this happens, it can be difficult to completely get rid of the cancer cells. This means that the tumor could grow back or become more aggressive. That’s why surgery is an important part of a patient’s treatment plan, but radiation therapy or chemotherapy might also be needed.
Because glioblastomas are more aggressive, they are often treated with a combination of radiation therapy and a low dose of chemotherapy. This is often followed by more chemotherapy.
Typically, other types of gliomas may be treated by radiation alone followed by chemotherapy. They might also be treated with different types of chemotherapy depending on the type of glioma. But they’re not usually treated with chemotherapy and radiation therapy together.
After completing treatment for glioma, patients undergo regular MRIs to make sure their tumor has not recurred. How often a patient is seen varies, depending on their diagnosis and treatment plan.
“There are many different types of gliomas, and our understanding of what makes certain ones act differently than others is continuing to evolve,” Aaroe says. “It’s important to make that distinction because these advances identify different prognoses and different optimal treatment options for patients.”
Request an appointment at MD Anderson online or by calling 1-866-553-0983.
Related Cancerwise Stories

Our understanding of what makes certain gliomas act differently than others is continuing to evolve.
Ashley Aaroe, M.D.
Physician