request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Glioblastoma
Glioblastoma is the most common primary brain cancer, or cancer that starts in the brain, with around 12,000 cases diagnosed in the United States each year. All glioblastomas are grade IV brain tumors, meaning they contain the most abnormal looking cells and are the most aggressive.
Glioblastoma is the most common primary brain cancer, or cancer that starts in the brain, with around 12,000 cases diagnosed in the United States each year. All glioblastomas are grade IV brain tumors, meaning they contain the most abnormal looking cells and are the most aggressive.
How does glioblastoma start?
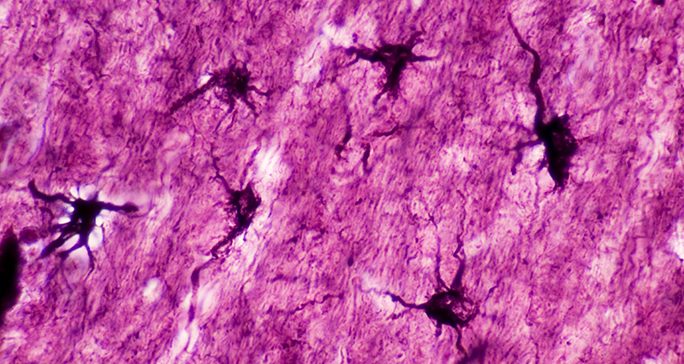
Glioblastoma begins in star-shaped brain cells called astrocytes that help protect the brain from diseases in the blood and provide it with nutrients.
Astrocytes are a type of glial cell. Glial cells supply the brain with nutrients and give the brain its shape. They also protect neurons from one other and create a stable chemical environment in the brain.
Glioblastoma most commonly begins near the forehead or near the bottom of the brain, although it can start anywhere in the brain. The area near the forehead is the frontal lobe. It plays important roles in speech, voluntary movement, behavior, and memory. The area near the bottom of the brain is the temporal lobe. It creates new memories, processes language, and processes input from the senses of hearing, sight, taste, and touch.
What’s the prognosis for glioblastoma?
There is currently no cure for glioblastoma. The median length of survival after a diagnosis is 15-18 months, while the disease’s five-year survival rate is around 10%. Though all glioblastomas recur, initial treatments may keep the tumor controlled for months or even years.
Glioblastoma statistics reflect many of the challenges in treating the disease.
As glioblastoma grows, it forms microscopic branches that can spread into different parts of the brain. These branches makes it nearly impossible to remove the entire tumor with surgery. In addition, a single tumor contains many different types of cells, so a drug that works for some cells may not successfully treat the entire tumor.
Brain tumors in general are hard to treat, as well. When removing tumors in other parts of the body, surgeons often take out a small section of healthy tissue surrounding the tumor, referred to as a margin. They do this to remove cancer cells that are not visible to the naked eye. Removing healthy brain tissue is much more difficult, since tissue near a tumor may control essential functions, such as speech, language and movement. During brain surgery, neurosurgeons strive to remove as much of the tumor as possible without damaging the parts of the brain that control these functions.
Delivering medications to the brain is also difficult. The blood vessels for the central nervous system (CNS) are designed to stop diseases and toxins in the blood from reaching this area, which includes the brain and spinal cord. Known as the blood brain barrier, this feature protects the brain, but it also stops many drugs from getting to brain tumors.
While glioblastoma is difficult to treat, clinical trials at MD Anderson are exploring new radiation therapy, chemotherapy and immunotherapy strategies to fight this disease. Other trials are designed to improve patients’ quality of life and lessen the burden of the disease and its treatments.
What are the risk factors for glioblastoma?
Anything that increases the chance of developing a particular disease is a risk factor.
Doctors have only identified a few risk factors for glioblastoma. The most significant is prior radiation to the head. People often receive radiation to the head to treat other cancers near the brain or cancers that have or may spread to the brain.
A few hereditary cancer syndromes are also connected to glioblastoma. These include Li Fraumeni syndrome, neurofibromatosis type 1 and Turcot syndrome.
In addition, this cancer tends to develop more often in men, people age 50 or older, and Caucasians.

MD Anderson is #1 in Cancer Care
Glioblastoma survivor: ‘MD Anderson is a blessing’
7 glioblastoma myths
What are the symptoms of glioblastoma?
Like all brain tumors, the symptoms of glioblastoma depend on the area of the brain where the tumor begins and spreads, as well as how quickly the tumor grows. Glioblastoma can:
- Invade and destroy brain tissue
- Put pressure on nearby tissue
- Take up space and increase pressure within the skull. This symptom is known as intracranial pressure.
- Cause fluids to accumulate in the brain tissue
- Block the normal circulation of cerebrospinal fluid through the spaces within the brain
- Cause bleeding
Brain tumor symptoms vary from person to person. They may include:
- Headaches: These are often the first symptoms of glioblastoma. Brain tumor headaches can differ from normal headaches. They typically become more frequent over time and may not respond to over-the-counter pain medicine. They may cause nausea or vomiting and can get worse when you lie down, bend over or bear down, such as when you have a bowel movement.
- Seizures: Seizures can take many different forms. While most people associate seizures with uncontrollable arm and leg movements and a loss of consciousness, symptoms can be subtler. Other seizure symptoms include numbness, tingling, difficulty speaking, strange smells or sensations, staring and unresponsive episodes.
- Changes in mental function, mood or personality: Brain tumors can cause people to become withdrawn, moody or inefficient at work. They may feel drowsy, confused and unable to think. Depression and anxiety, especially if either develops suddenly, may be an early symptom of a brain tumor. Brain tumors may also cause behavior changes, including a loss of inhibitions.
- Changes in speech: People with brain tumors may have trouble finding words, speak incoherently, and be unable to express or understand language.
- Sensory changes: Changes in the ability to hear, smell or see, including double or blurred vision can be symptoms of a brain tumor. The sense of touch can also be impacted. People with brain tumors may lose some of their ability to feel heat, cold, pressure, sharp edges or light touches.
- Loss of balance or coordination
- Changes in pulse and breathing rates: This symptom usually occurs with a brain tumor compresses the brain stem, which controls basic bodily functions including breathing and the heart rate.
These symptoms do not always mean you have a brain tumor. However, it is important to discuss any symptoms with your doctor, since they may signal other health problems.
How is glioblastoma diagnosed?
If you have a brain tumor, it is important to get the most accurate diagnosis possible. This will help your doctor pinpoint the tumor to give you the most advanced treatment with the least impact on your body.
At MD Anderson, we have the most sophisticated equipment available to identify brain tumors and find out exactly how far they may have spread in the central nervous system.
Our specialized staff truly sets us apart. The Brain and Spine Center has renowned neuropathologists who focus solely on diagnosing brain and spine tumors.
These experts were instrumental in writing the World Health Organization book that defines every type of brain tumor and provides standard classifications for doctors worldwide. When called on to give a second opinion, they change diagnoses for up to 10% of patients first diagnosed at another hospital. Their expertise and experience can make a big difference in brain tumor treatment success.
Glioblastoma diagnostic tests
The process of diagnosing glioblastoma is essentially the same as testing for other brain tumors.
If you have symptoms that signal a brain tumor, your doctor will examine you and ask questions about your health, your lifestyle and your family’s medical history.
If the doctor decides further testing is needed, he or she will order an imaging exam. One or more of the following tests may be used to find out if you have a brain tumor. These tests also may be used to find out if treatment is working.
Imaging exams: Imaging exams let doctors see tumors in and around the brain. Glioblastoma imaging exams include:
- CT (computed tomography) scans
- MRI (magnetic resonance imaging)
- ABTI (advanced brain tumor imaging): This imaging technique provides doctors with highly detailed information on the tumor. It is used to evaluate new tumors, identify recurrence and guide treatment decisions.
Biopsy: While imaging tests may show an area where there could be a brain tumor, doctors need a tissue sample to definitively diagnose a primary brain tumor. Tissue samples are obtained by a biopsy. For glioblastoma, a tissue sample is usually retrieved during surgery to remove the tumor. A pathologist will then examine the cells to make a diagnosis. Since glioblastoma is a very complex disease, it is best to work with a pathologist with extensive experience in diagnosing brain cancers to get an accurate diagnosis from the very beginning.
Molecular testing: Some primary brain tumors, including glioblastoma, are defined by their key molecular features that are results of mutations in the tumor. These features can be used to diagnose a tumor, provide a more accurate prognosis and enhance the treatment plan. This is an area of ongoing study and more mutations will almost certainly emerge. Currently, the key molecular subtypes of glioblastoma include:
- IDH mutation: IDH is a gene that produces proteins that help repair damaged DNA. In general, patients whose tumor has an IDH mutation have a better prognosis than those who do not have the mutation (known as IDH wildtype). Doctors believe this is because the mutation limits the ability of IDH proteins to repair cancer cell DNA.
- MGMT promoter methylation: MGMT is an enzyme that can make cancer cells more resistant to therapy. When the DNA associated with producing this enzyme is mutated through a process called methylation, less MGMT is made. Glioblastoma with the MGMT promoter methylation mutation may respond better to treatment. Testing for the MGMT mutation is required for many brain tumor clinical trials.
What are the treatment options for glioblastoma?
At MD Anderson’s Brain and Spine Center, some of the nation’s leading glioblastoma experts will develop your treatment plan based on your specific needs. They take a team approach, with neurosurgeons, neuro-oncologists and radiation oncologists working together to coordinate your care and deliver the best therapies with the fewest side effects. Your quality of life is also a key concern during treatment, and our care team constantly looks for ways to make patients as comfortable and self-sufficient as possible.
Glioblastoma treatment plan
The standard treatment for glioblastoma starts with surgery to remove as much of the tumor as safely as possible.
Surgery typically does not remove all of the tumor, though. This is because glioblastoma usually forms microscopic branches that spread into different parts of the brain.
After surgery, patients usually get a combination of chemotherapy and radiation therapy, followed by chemotherapy alone. Elderly patients and/or those who have little to no ability to care for themselves (such as bathing, dressing or feeding themselves) may not be able to withstand the combined chemotherapy and radiation therapy phase of treatment. In these cases, they may receive a modified combination or just one of the two therapies.
Glioblastoma surgery
Glioblastoma surgery is most successful when it’s performed by a neurosurgeon with extensive experience in brain tumor surgery. MD Anderson neurosurgeons are world renowned leaders in their field, with extensive experience operating on glioblastoma tumors.
At MD Anderson’s Brain and Spine Center, these surgeons have access to the most advanced surgical technologies in the world.
Among these technologies is the Brainsuite® intraoperative MRI, found in just a handful of hospitals around country. This technology images the brain during surgery, helping neurosurgeons safely remove as much of the tumor as possible. Our neurosurgeons also have access to functional magnetic resonance imaging (fMRI) and navigated transcranial magnetic stimulation (nTMS). These technologies highlight key areas of speech and motor function in the brain, helping surgeons plan their procedures.
There are a number of different surgical options for people with glioblastoma. Your physician will evaluate your case and discuss the best one for you.
Craniotomy
Craniotomies are the standard surgery for most brain tumors, including glioblastoma. Surgeons performing a craniotomy remove a section of the skull in order to access the tumor.
Awake craniotomy
One advanced type of surgery offered at MD Anderson is the awake craniotomy. This procedure is performed on patients whose tumor is located in a part of the brain that controls essential functions. During an awake craniotomy, doctors wake up the patient during the procedure. They can then interact with the patient to map the location of key areas of the brain. This lets the neurosurgeon avoid those functional areas during surgery while removing as much of the tumor as safely as possible. Because of local anesthesia and the brain’s lack of pain receptors, patients don’t feel any pain during the operation.
This is a highly specialized procedure that is only performed at a handful of hospitals across the country. Combined, the neurosurgeons at MD Anderson perform roughly two awake craniotomies a week, making them among the most experienced surgeons in the world for performing this procedure.
Laser interstitial thermal therapy
This treatment, also known as LITT, is primarily used to treat tumors that are difficult to reach with standard surgical techniques. During the procedure, neurosurgeons use an intraoperative MRI in an advanced operating room called the BrainSuite® to guide a small laser catheter to the tumor site. There, the laser heats the tumor, killing cancerous cells from the inside while minimizing damage to nearby healthy brain cells.
Radiation therapy for glioblastoma
Radiation therapy uses focused, high-energy beams to kill tumors or tumor sections that cannot be removed with surgery. MD Anderson offers the most advanced radiation therapy techniques in the world. Each radiation plan is designed to have the maximum impact on the patient’s tumor while minimizing the effect on healthy brain tissue. The different radiation therapies used to treat glioblastoma are described below. Your radiation oncologist will evaluate your condition and recommend the one that is best for you.
3D conformal radiation therapy for glioblastoma
This technique uses three-dimensional scans to determine the exact shape and size of the tumor. Tiny metal leaves inside the treatment machine, called a linear accelerator, are used to shape the radiation beams. These beams are designed to match the size and shape of the tumor, which minimizes radiation exposure to nearby healthy tissue.
Intensity modulated radiation therapy (IMRT) for glioblastoma
IMRT focuses multiple beams of radiation with different intensity levels directly on the tumor, delivering the highest possible dose of radiation. Radiation oncologists at MD Anderson use special software to develop highly-targeted radiation treatment plans for each patient that minimizes the impact on healthy tissues near the tumor.
Proton therapy for glioblastoma
Proton therapy is a specialized form of radiation therapy that delivers high doses of energy directly to the tumor site, with minimal impact on healthy tissue. It is only available at a few centers in the world and is often used to treat tumors located in very sensitive areas of the brain. Proton therapy is currently considered experimental for glioblastoma and would be recommended only as part of a clinical trial.
Stereotactic radiosurgery for glioblastoma
Stereotactic radiosurgery (SRS) is a non-invasive treatment that uses dozens of tiny radiation beams to accurately target brain tumors with a single high dose of radiation. Despite its name, SRS is not a surgical procedure and does not require an incision or anesthesia. This technique is typically used for patients whose tumors have recurred and who have already received standard radiation treatments.
Chemotherapy for glioblastoma
Chemotherapies are drugs that kill fast-growing cells, including cancer cells. MD Anderson has the most advanced chemotherapies for glioblastoma available.
Chemotherapy can be difficult to deliver to the brain because of the blood-brain barrier, a set of small blood vessels and brain cells that protect the brain from disease, but also act as a shield against chemotherapy drugs.
Tumor treating fields for glioblastoma
This treatment requires patients to shave their heads and wear an adhesive skull cap with wires attached to a battery pack for 18 hours a day. During these hours, the device emits radio waves into the brain in order to slow or stop tumor cells from multiplying.
Glioblastoma clinical trials
Because glioblastoma is difficult to treat, doctors are constantly searching for new ways to fight the disease. MD Anderson has one of the most active glioblastoma clinical trials programs in the world. Some trials study entirely new treatments, while others look at new combinations of existing treatments that may benefit patients. Many use personalized approaches designed around the specific features of a patient’s cancer.
These include trials of surgeries, chemotherapies and radiation therapies. Doctors are also working to bring the latest breakthroughs in cancer care to glioblastoma treatments, including new targeted therapies and immunotherapies. Visit our clinical trials site to search for glioblastoma clinical trials.
Read more:
Recurrent glioblastoma treatment
Because it is impossible to remove or destroy all glioblastoma cells in a tumor, all glioblastomas recur. The timing can range from weeks to years.
Some patients with recurrent glioblastoma may be eligible for another surgery or LITT to remove as much of the tumor as possible. Radiation therapy can also be used as a palliative measure to slow tumor progression and to relieve symptoms caused by the tumor.
However, many standard treatments haven’t proven effective for recurrent glioblastoma. Patients should work with their care team to consider available treatment options and choose a plan that meets their goals. Many clinical trials are available for recurrent glioblastoma, and MD Anderson has one of the largest glioblastoma clinical trial programs in the country, including trials that offer personalized care built around the characteristics of the patient’s specific disease.
Why Choose MD Anderson for glioblastoma care?
After learning they have a brain tumor, many people feel they must schedule surgery as soon as possible. However, most brain tumor patients, including those with glioblastoma, have time to research their options.
As MD Anderson neurosurgeons have shown, removing as much of the tumor as possible, known as maximal safe resection, during the first surgery leads to better survival for glioblastoma patients. Choosing the right hospital for your first surgery or treatment is one of the most important decisions you can make as a glioblastoma patient.
Because this is a difficult cancer to treat, finding doctors with experience and expertise in treating glioblastoma is key. At MD Anderson Cancer Center, we have many of the world leaders in glioblastoma care, including top neurosurgeons, neuro-oncologists and radiation oncologists who specialize in the central nervous system. In most cases, the experts at MD Anderson are able to identify the unique characteristics of the patient's glioblastoma on a molecular level. This information may support the creation of a personalized treatment plan tailored specifically to the patient’s disease.
As a top-ranked cancer hospital, MD Anderson also is home to one of the world’s largest collections of glioblastoma clinical trials designed to improve outcomes for patients. These trials include studies of new chemotherapies, radiation therapies and immunotherapies, among other treatments.
In addition to treating the disease directly, MD Anderson’s Brain and Spine Center offers leading neuropsychology care. We monitor the impact of the disease and its treatments on patients’ cognitive health. If needed, we can adjust treatments to improve patients’ quality of life and ability to function day-to-day.
Some glioblastoma treatments are even offered beyond MD Anderson’s campus in the Texas Medical Center. Through our five Houston-area locations, glioblastoma patients throughout the region may be able to receive radiation therapy or chemotherapy from MD Anderson physicians close to home.
You've got to believe in yourself and believe that you will beat this cancer.
Nicole Adams
Survivor
Treatment at MD Anderson
Glioblastoma is treated at our Brain and Spine Center and Proton Therapy Center

Clinical Trials
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
MyCancerConnection
Prevention & Screening
Counseling
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.