- Diseases
- Acoustic Neuroma (16)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (18)
- Bile Duct Cancer (26)
- Bladder Cancer (74)
- Brain Metastases (28)
- Brain Tumor (234)
- Breast Cancer (726)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (168)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (130)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (178)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (150)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (300)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (100)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (22)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (238)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (122)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (936)
- Research (390)
- Second Opinion (78)
- Sexuality (16)
- Side Effects (616)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (408)
- Survivorship (328)
- Symptoms (182)
- Treatment (1788)
What causes jaundice in adults?
3 minute read | Published August 26, 2024
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on August 26, 2024
Jaundice is a yellowing of the skin and eyes caused by abnormally high levels of bilirubin, an orangey-yellow pigment found in a liver secretion called bile.
In newborns, jaundice generally occurs because the liver is not fully developed. But in adults, it’s often a sign that something is wrong.
How long jaundice may last depends on its source. Read on to learn more about this symptom of many gastrointestinal cancers, as well as which non-cancerous conditions can cause it and when to see a doctor.
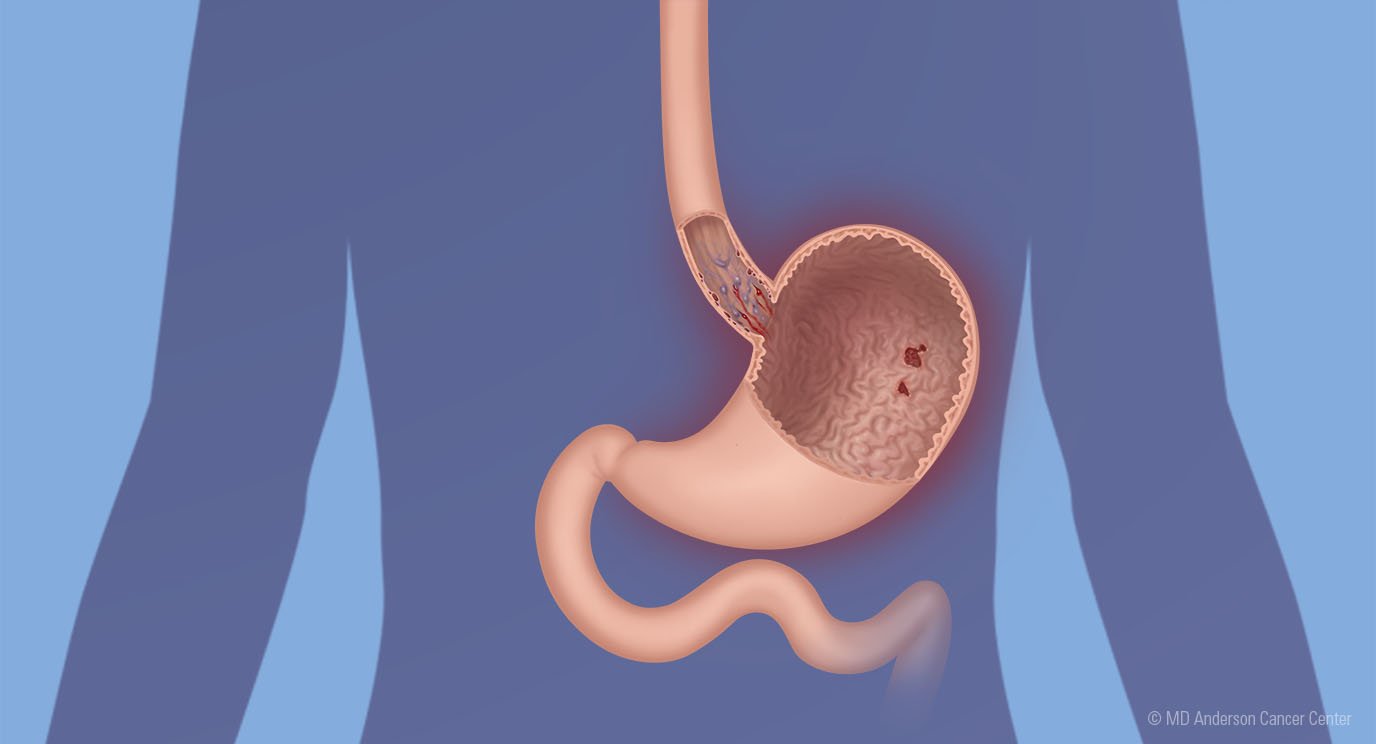
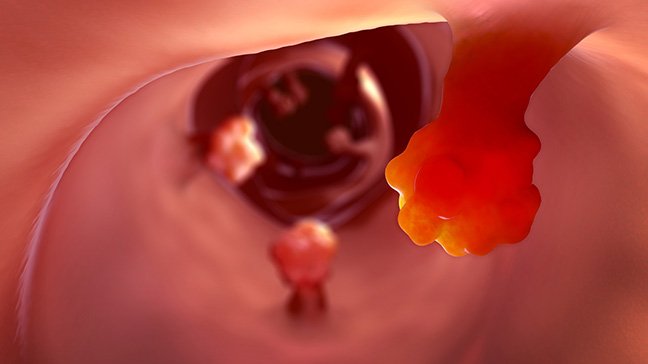
Many gastrointestinal cancers can cause jaundice
In adults, jaundice may be a symptom of:
- liver cancer
- pancreatic cancer
- bile duct cancer
- gallbladder cancer
- ampullary cancer
- stomach cancer
- cancer that originates elsewhere, but spreads to the liver, pancreas, bile duct or gallbladder
- diffuse large B-cell lymphoma
With lymphoma, jaundice is usually related to the breakdown of blood cells. But in most other cases, it’s either due to an obstruction or to the malfunction of the liver.
With obstructive jaundice, the outflow of the liver’s secretions is being blocked, so the bilirubin backs up. With malfunction-related jaundice, the liver is not working properly. This could be due either to liver failure or to liver disease, such as cirrhosis or hepatitis.
Anything that blocks the bile duct or takes up a significant amount of space in the liver can cause jaundice. But it’s most frequently seen with liver and pancreatic cancers.
Typically, jaundice is also seen when cancer is at a more advanced stage. But depending on where a tumor is located, it could be an early sign, too. Even a small tumor on the head of the pancreas can cause scarring and lead to obstruction.
What jaundice looks like
A lot of people think of yellow skin or eyes when you first mention jaundice. While jaundice does occur in those locations, it usually starts under the tongue. You may notice it there first, then in the whites of your eyes and finally, on your skin.
But the early stages of jaundice can be pretty subtle, so people don’t normally notice it themselves. Usually, a loved one is the first person to say, “Hey, I think you’re turning yellow.” In jaundice’s latter stages, though, people can practically glow in the dark.
Other symptoms of liver dysfunction can accompany jaundice
Jaundice is typically the main sign that something is wrong with the liver. But in some cases, you might notice other symptoms, such as itchy skin or changes in urine color. With obstructive jaundice, bilirubin can become so backed up that it starts spilling out into the bladder, making the urine very dark.
Occasionally, though, patients will go in for a regular exam, and lab tests will show that their bilirubin levels are slightly elevated. That might not be enough for jaundice to be visible yet, but it will still prompt an additional evaluation.
When to see a doctor about jaundice
There are many reasons you might develop jaundice that are unrelated to cancer. These include:
- hepatitis
- infection
- Gilbert syndrome (a benign condition seen in about 5% of the population)
- dehydration (very rarely)
Some are benign conditions that can cause slightly elevated bilirubin levels. But none of them are normal.
So, if you’re turning yellow, something’s wrong, and you should see a doctor pretty quickly to find out why. Any amount of jaundice should prompt a clinical evaluation.
Matthew Katz, M.D., is chair of the Department of Surgical Oncology at MD Anderson.
Request an appointment at MD Anderson online or call 1-877-632-6789.

Any amount of jaundice should prompt a clinical evaluation.
Matthew Katz, M.D.
Physician