request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Pancreatic Cancer
Get details about our clinical trials that are currently enrolling patients.
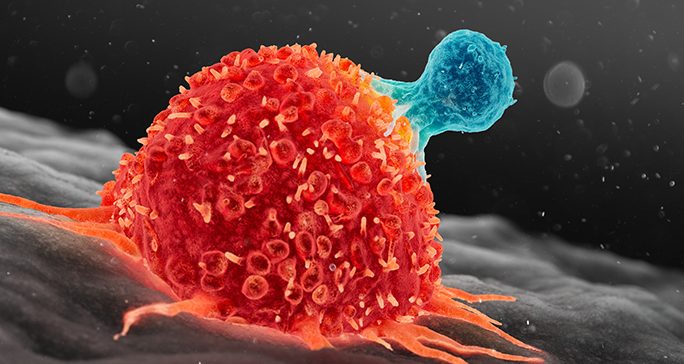
View Clinical TrialsPancreatic cancer occurs when cancer cells form and grow within the pancreas. These tumors are hard to diagnose early, since pancreatic cancer signs and symptoms aren’t obvious. Because of this, the majority of these cancers are diagnosed after the disease has reached an advanced stage, when treatment options are limited.
Pancreatic cancer occurs when cancer cells form and grow within the pancreas. These tumors are hard to diagnose early, since pancreatic cancer signs and symptoms aren’t obvious. Because of this, the majority of these cancers are diagnosed after the disease has reached an advanced stage, when treatment options are limited.
Pancreatic cancer is the third leading cause of cancer death in the United States. It is estimated that close to 60,000 new cases are diagnosed each year and over 47,000 people die because of this disease annually. The lifetime risk of developing the disease is 1.6%. The risk is slightly higher for men than women and the typical age range at the time of diagnosis is between 65-74 years old.
About the pancreas
The pancreas is an oblong organ located behind the lower part of the stomach, between the stomach and the spine. It produces juices that aid in digestion and makes insulin and other hormones that help the body absorb sugar and control blood sugar.
The pancreas mainly contains two kinds of cells:
- Exocrine cells, which make and release enzymes that aid in food digestion.
- Endocrine cells, which produce and release important hormones directly into the bloodstream.
The majority of pancreatic cancers start in the exocrine cells that line the ducts of the pancreas. These are called pancreatic adenocarcinomas.
When cancer begins in pancreatic endocrine cells, it’s called a pancreatic neuroendocrine tumor (NET). There are many subtypes of this type of tumor.
This summary is about exocrine pancreatic cancer. Further mention of pancreatic cancer refers only to pancreatic adenocarcinoma, and not pancreatic NETs.
Pancreatic cancer risk factors
Anything that increases your chance of developing pancreatic cancer is a risk factor. Some risk factors can be changed, while others cannot.
Risk factors that can be changed include:
- Smoking and tobacco use: People who smoke are about twice as likely to develop pancreatic cancer.
- Obesity: Being very overweight (having an elevated body mass index, or BMI) increases your chance of developing pancreatic cancer by 20%.
Other pancreatic cancer risk factors can’t be changed, including:
- Age: The risk of pancreatic cancer increases sharply after 55 years old.
- Race: African-Americans are more likely to have pancreatic cancer than other ethnic groups.
- Family history: Hereditary genetic changes may account for about 10% of pancreatic cancers. Examples of genetic syndromes that can cause exocrine pancreatic cancer include: Hereditary breast and ovarian cancer syndrome caused by mutations in the BRCA1 or BRCA2 genes, Lynch syndrome (usually defects in MLH1 or MSH 2 genes), and hereditary pancreatitis due to mutations in PRSSI gene.
- Diabetes: People with long-standing history of type 2 diabetes have an increased likelihood of developing pancreatic cancer.
- Chronic pancreatitis: Long-term inflammation of the pancreas is linked with increased pancreatic cancer risk, especially in smokers.
Not everyone with the above risk factors gets pancreatic cancer. However, if you have risk factors, you should discuss them with your doctor.
Learn more about pancreatic cancer:

MD Anderson is #1 in Cancer Care

‘How I knew I had pancreatic cancer’: Survivors share their...
Why choose MD Anderson for pancreatic cancer treatment?
About 80% of pancreatic cancers are diagnosed after the disease has reached an advanced stage, which makes them hard to treat. Less than 20% of pancreatic cancers are caught when the cancer is still confined to the pancreas or closely surrounding areas. Though the disease has not spread, these cases are treated with complicated surgical operations that require a high level of experience to perform safely and effectively.
Whether you’re diagnosed with localized or metastatic pancreatic cancer, it’s important to find a team of physicians with the most innovative treatment options and expertise. At MD Anderson, you are the focus of a personalized pancreatic cancer treatment plan that brings together a multidisciplinary team of some of the top pancreatic cancer professionals that use the most advanced techniques.
World-class surgeons treating localized pancreatic cancer
When pancreatic cancer is confined to the pancreas, and sometimes when it has spread only to the nearby areas, it can be removed with surgery. The highest chances for successful treatment occur when the tumor is completely removed, and the surgical techniques required are extremely complex. Because our surgeons are among the most experienced and skilled in the nation, MD Anderson has:
- The highest 5-year survival rate reported in the surgical literature for patients who have undergone surgery for pancreatic cancer.
- Less than a 1% mortality rate after surgery. That is over 6% lower than the national average.
- Among the shortest average length of hospital stay after surgery.
Pioneers of pancreatic cancer treatment
Our experts provide comprehensive pancreatic cancer care, and they have pioneered several advances in the field, including:
- The use of chemotherapy and/or radiation in the preoperative setting.
- Establishment of the “borderline resectable” staging subgroup and definition of the best course of treatment. Incorporating this staging group leads to larger numbers of patients with advanced cancer that may benefit from combining several types of therapy, including surgery.
- Innovative radiation techniques, such as giving higher-than-normal doses of radiation therapy (dose escalation) and stereotactic body radiation therapy (SBRT).
Developing more effective treatment options through clinical trials
MD Anderson conducts a wide range of clinical trials to test new and innovative treatment options for both localized and metastatic pancreatic cancer. The treatment options used in these trials often cannot be found anywhere else and are critical for advancing pancreatic cancer treatment.
Current clinical trials focus on:
- Combining several types of therapy before surgery to treat resectable and borderline resectable pancreatic cancer.
- Identifying more effective ways to use chemotherapy and radiation therapy to treat pancreatic cancer tumors that can’t be removed surgically.
- Developing more effective treatment options for pancreatic cancers that have metastasized.
- Detecting pancreatic cancer earlier (especially in patients with risk factors).
- Promoting healthy habits that enhance the effectiveness of treatment.
Learn more about our pancreatic cancer clinical trials and research.
Offering the latest radiation therapy techniques
Radiation therapy can be a powerful tool in pancreatic cancer treatment. Our radiation oncologists are experts at stereotactic body radiation therapy (SBRT) and dose-escalation, which allow high doses of radiation to be delivered to the tumor without damaging healthy tissue. Many MD Anderson faculty have led or are leading national clinical trials to improve radiation therapy for pancreatic cancer.
Did You Know
Treatment at MD Anderson
Pancreatic cancer treated in our Gastrointestinal Center.

Featured Articles
Exploring pancreatic cancer vaccines: What’s next?

Pancreatic cancer survivor finds hope in cancer research

Pancreatic cancer survivor: I’m glad I took a chance on a...

Chief Patient Experience Officer: My pancreatic cancer diagnosis...

Husband and wife undergo same pancreatic cancer surgery

Pancreatic cyst and cancer survivor: Why I’m glad I went to MD...

Pancreatic cysts: What they are and how they’re treated

Pain management for pancreatic cancer patients
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention & Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.

