- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (160)
- Colon Cancer (166)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (82)
- Vaginal Cancer (18)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (632)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (920)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (608)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (322)
- Symptoms (182)
- Treatment (1786)
Stereotactic body radiation therapy: a new option for pancreatic cancer patients
BY Devon Carter
4 minute read | Published October 18, 2018
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on October 18, 2018
A decade ago, pancreatic cancer was treated with five to six weeks of radiation therapy and chemotherapy. Patients often experienced side effects that drastically impacted their quality of life and saw little survival benefit.
But a type of radiation therapy called stereotactic body radiation therapy (SBRT) is now offering some pancreatic cancer patients a better option. We spoke with Cullen Taniguchi, M.D., Ph.D., to learn more.
What makes stereotactic body radiation therapy different?
Standard radiation therapies use a wider beam with a lower dose over a longer period of time. But SBRT is like a laser beam. We can deliver a more precise, higher dose of radiation in a shorter amount of time. So, whereas standard radiation therapy requires weeks of treatment, SBRT requires only five days, preferably consecutively. And each session is about 40 minutes, so there’s much less disruption to patients’ lives.
Also, because SBRT is so effective, it may reduce the need for long-term chemotherapy for some patients.
How is stereotactic body radiation therapy more precise?
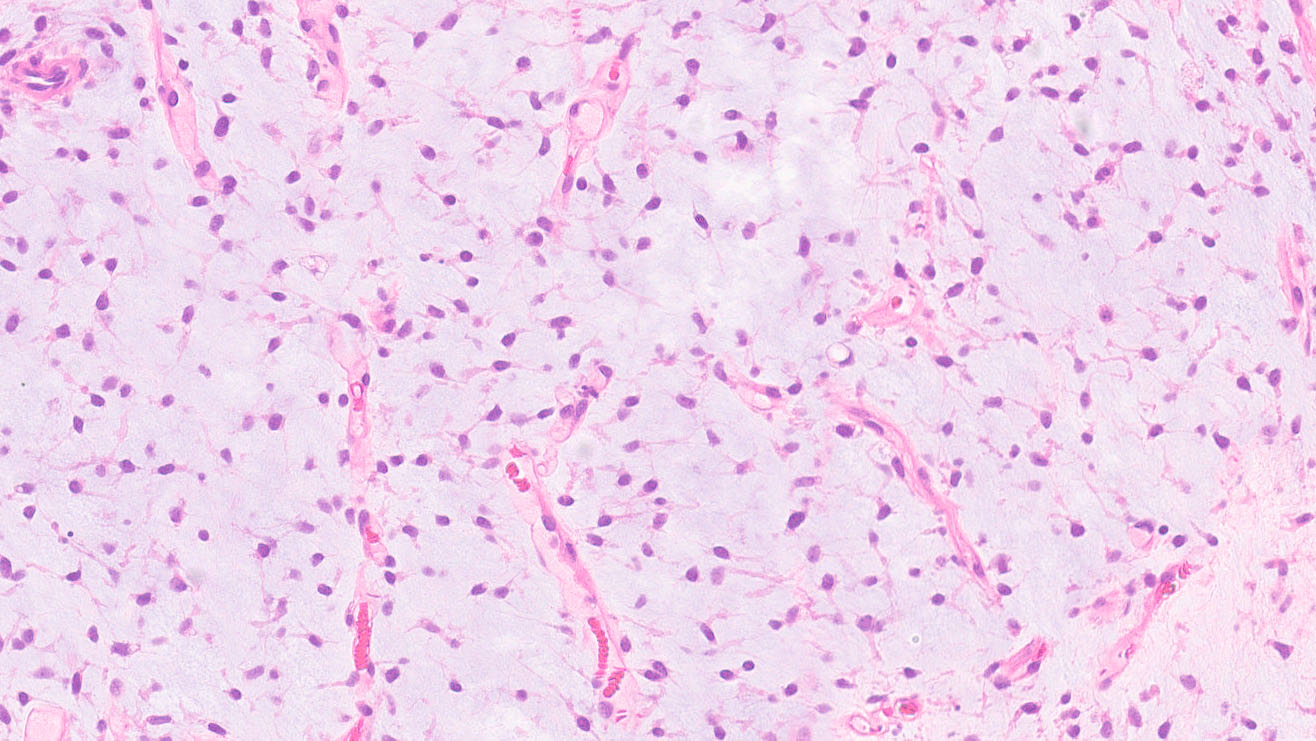
SBRT has a narrower beam of radiation that allows us to more precisely target the tumor.
Also, when a patient breathes, the tumor moves about a centimeter. To protect normal tissues from radiation exposure, we can track the tumor’s movement during breathing and activate the radiation beam only when the body is in a certain position. Or we can have the patient hold his or her breath for a few seconds and radiate the tumor when the body is still.
And to better target the radiation beam, we can implant two or three fiducials, which are gold markers the size of rice kernels. They’re inserted directly into or near the tumor endoscopically in an outpatient procedure that’s similar to a biopsy. They remain in the body unless the tumor is removed surgically after radiation. They make treatment more effective by helping ensure we destroy the tumor without harming any nearby tissues.
What are the side effects of stereotactic body radiation therapy?
Because SBRT is such a short course of radiation, patients don’t experience many side effects like they do with other radiation therapies. For instance, patients don’t have skin changes and only a few experience nausea. However, there’s a slightly higher risk of development of ulcers in the bowel, which may show up around three months after the treatment is complete.
How can these side effects be minimized?
We’re very careful when identifying patients who should receive SBRT to ensure that these patients aren’t at high risk for these long-term complications. For instance, SBRT is not the best option for a patient whose tumor is close to the bowel or stomach. If the tumor responds too quickly to the treatment, it can leave a hole in the digestive system. Because we better select patients based on this knowledge, we’ve been able to reduce the risk of ulcers from 10% to less than 2%.
Who’s a good candidate for SBRT?
Because stereotactic body radiation therapy delivers such a high dose of radiation and we want to limit radiation exposure, the best candidates are patients whose cancer hasn’t spread beyond the pancreas.
SBRT may also be a good option for patients who may not be candidates for surgery because their localized pancreatic tumor is touching a blood vessel. By shrinking the tumor with SBRT first, we’re able to offer surgery to more patients. And of the patients that receive surgery, we can successfully remove the entire tumor in 90% of patients, which reduces their risk of the cancer coming back.
But if a patient isn’t well-suited for surgery, SBRT can still be an option. It can help stabilize the growth of the tumor and prevent it from causing an obstruction in the bowel.
What stereotactic body radiation therapy research is underway?
We’re examining if we can safely give a higher dose to reduce the treatment time even further. If that’s not feasible, we’re studying whether there’s a drug that allows us to give a lower dose of radiation but with better results.
Additionally, I'm leading a clinical trial that’s exploring raising the SBRT dosage while minimizing the risk of ulcers with the use of a potential radiation protector in pancreatic cancer patients.
We’re also combining SBRT with other therapies. For example, we’re studying if immunotherapy can jumpstart the immune system’s reaction to a tumor and make radiation therapy more effective. We’re also exploring targeted therapies to see if they will make a tumor respond better to radiation therapy.
Lastly, we have a clinical trial that is looking at whether changing a patient’s microbiome can improve responses to radiation therapy.
What’s your advice for pancreatic cancer patients?
As doctors and researchers, we’re really excited about using stereotactic body radiation therapy to treat pancreatic cancer. Because we’re able to treat these challenging tumors with more precision in less time, we’re seeing our patients live longer with fewer complications. That’s incredibly rewarding.
But if you’re considering SBRT, choose a cancer center like MD Anderson that specializes in it for pancreatic cancer. It’s a relatively new therapy that’s just being expanded to treat this difficult disease. And it’s not just the doctor’s expertise that counts. Look for a whole team that’s experienced to ensure you’re getting the best treatment possible for the best possible outcome.
Request an appointment at MD Anderson online or by calling 1-866-230-7585.