- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (722)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (176)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (148)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (298)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (236)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (928)
- Research (388)
- Second Opinion (76)
- Sexuality (16)
- Side Effects (614)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (324)
- Symptoms (182)
- Treatment (1778)
Stage IV leiomyosarcoma survivor: Faith and quality care got me through cancer
5 minute read | Published October 31, 2024
Medically Reviewed | Last reviewed by Maria Zarzour, M.D., on October 31, 2024
Sheri Peters was diagnosed with stage IV leiomyosarcoma of the uterus in 2015. Her 17-year-old son, Zach, had died from stage IV Ewing’s sarcoma just three years earlier.
Sheri had relied on her faith to get through the loss of her son. She leaned on her faith again as she faced her own diagnosis.
Symptom that led to leiomyosarcoma diagnosis
At age 52, Sheri began to bleed heavily. She figured it was part of menopause and continued with her normal activities – walking, jumping on her outdoor trampoline and teaching at a local high school. But the bleeding got worse.
“I would see clumps while taking a shower,” she recalls. “I knew it wasn’t normal. I’d even passed out from the bleeding.”
Sheri’s husband, Leonard, took her to the hospital. An ultrasound showed she had a huge fibroid, which the doctor believed was causing the bleeding. She got a blood transfusion. But that only offered temporary relief.
“Leonard and my primary care doctor wanted me to get a hysterectomy to stop the bleeding,” says Sheri, who hesitated at first. “I wanted to make sure I was there to help my students prepare for their tests. But when the bleeding continued to get worse, I decided to have the hysterectomy.”
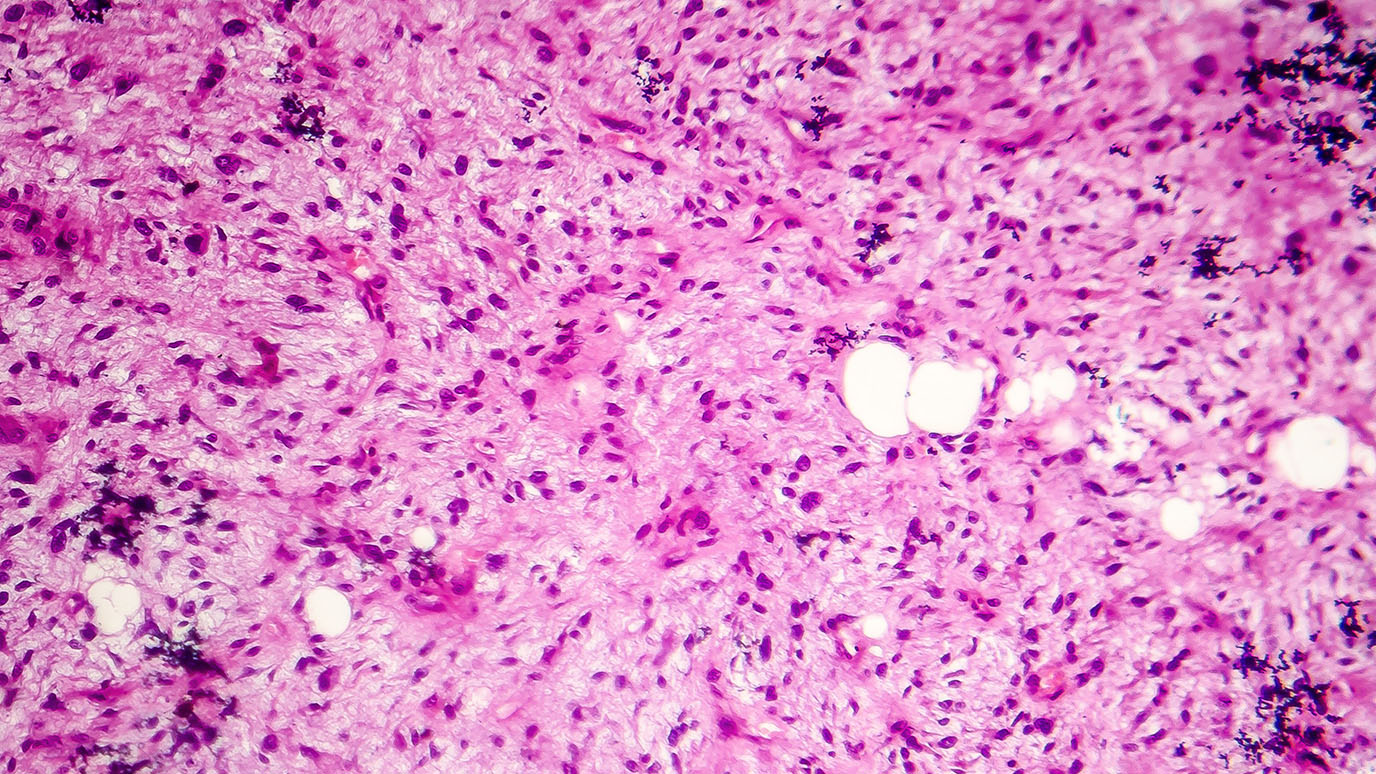
In early June 2015, Sheri underwent surgery to remove her uterus. Her gynecologist sent samples of the fibroid to pathology for a biopsy.
“We waited for 12 days for the pathology report,” recalls Sheri. “I remember telling Leonard that something was wrong. It shouldn’t take that long.”
When her doctor called and told her to come in right away, Sheri suspected she might be dealing with more than just a fibroid.
“He showed us the pathology report and said the pathologist had sent it to six other pathologists to verify the diagnosis because it was so rare,” Sheri recalls.
It was leiomyosarcoma. The tumor was six inches long. Sheri’s doctor immediately suggested she go to MD Anderson for treatment. It was a familiar place for Sheri, whose son had been treated here.
Starting leiomyosarcoma treatment at MD Anderson
Sheri saw a gynecologist at MD Anderson who said large tumors have a high chance of spreading to other parts of the body. She had a CT scan the next day to see if the cancer had spread.
Two days after that, Sheri met with sarcoma medical oncologist Maria Zarzour, M.D., and her physician assistant, Elizabeth Gilbert (now Urquiola).
A CT scan of the chest showed that the cancer had spread to her lungs. That meant it was stage IV.
“Dr. Zarzour said I had too many tumors to count, some of them the size of a quarter,” Sheri recalls. “Because the cancer was so aggressive and advanced, the average lifespan I had after diagnosis was 18 months. I even asked Dr. Zarzour how long I would have had if I hadn’t done anything at all. Her estimate was about six months.”
Sheri’s treatment was a combination of the chemotherapy drugs doxorubicin and ifosfamide. She had a central venous catheter placed in her chest, so the drugs were delivered directly to her bloodstream.
“Dr. Zarzour said if my tumors remained stable, she would be excited,” says Sheri. “If they shrank a little, she would be over the moon. And if they disappeared completely, she would dance.”
In August, a scan showed that the tumors were responding well to treatment. Some that were the size of a quarter had shrunk by 75%, others by 66%, and some of the smaller ones disappeared altogether.
“Every scan I had showed progress. More tumors were disappearing,” she says. “I’d always tell Dr. Zarzour, ‘You’re going to dance!’”
Leaning into faith and trusting her care team
During treatment, Sheri developed painful sores near her rectum. Leonard took her to MD Anderson’s Acute Cancer Care Center when she started running a fever.
“They explained that the sores were a side effect from treatment and would go away once I finished chemo,” says Sheri. “They kept me in the hospital for a week to treat a secondary infection to chemo. The chemo lowered my white blood cell count, which made me more susceptible to infection. They said I was the only sarcoma patient on chemo who pushed the pole around the hospital floor. I was determined to stay active!”
Because the chemo caused a significant drop in Sheri’s blood cell counts, Zarzour reduced the dosage. Then she decided to split up the drugs so that Sheri would not be taking doxorubicin and ifosfamide at the same time.
“She stopped the chemo for about five weeks because she didn’t want my counts to be completely wiped out to where they wouldn’t recover,” says Sheri.
She returned home depressed, afraid that she wouldn’t be able to continue treatment.
“I knew they could not cure me, only extend my days,” she says. “I watched my son go through treatment, so I knew the hard side of cancer. I cried and prayed for healing. And then I decided to just trust in God.”
Sheri was cleared for another round of chemotherapy in early November. She took doxorubicin.
“Three weeks later, I’m nervously waiting in the room for my scan results,” she recalls. “I’d gone through five weeks of no chemo and wondered if cancer had gotten the upper hand.”
But when Zarzour entered the room, she was dancing.
“She told me I’d beaten the odds. My cancer was gone!” recalls Sheri. “My family and I were overwhelmed with joy and gratitude. I had one more infusion of each chemotherapy drug in December, and then I was done.”
Grateful to be cancer-free
For three years, the cancer did not grow. Then, in 2019, thoracic surgeon Ara Vaporciyan, M.D., removed a small tumor on Sheri’s right lung. And in 2021, he removed a small tumor on the left lung. There has been no growth of the cancer since.
Sheri comes to MD Anderson every five months for checkups. She doesn’t take it for granted that she went from having 18 months to live after her initial diagnosis to now surpassing nine years.
She offers some advice to people who’ve recently received an advanced cancer diagnosis:
“Lean into your faith. This will provide you with strength, courage and peace of mind.”
She stresses the importance of finding a strong support system. “You’ll need people who can take you to and from appointments and encourage you when it gets hard.”
And seek the best care possible. “Go to the very best for treatment. For me, that was MD Anderson. They have one of the best sarcoma units in the country, if not the world. I trust my doctors completely. They care about me and know what they’re doing.”
Request an appointment at MD Anderson online or call 1-877-632-6789.

Go to the very best for treatment. For me, that was MD Anderson.
Sheri Peters
Survivor