- Diseases
- Acoustic Neuroma (16)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (18)
- Bile Duct Cancer (26)
- Bladder Cancer (74)
- Brain Metastases (28)
- Brain Tumor (234)
- Breast Cancer (728)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (168)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (130)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (178)
- Pancreatic Cancer (162)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (150)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (302)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (100)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (22)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (240)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (122)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (940)
- Research (390)
- Second Opinion (78)
- Sexuality (16)
- Side Effects (616)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (408)
- Survivorship (330)
- Symptoms (182)
- Treatment (1794)
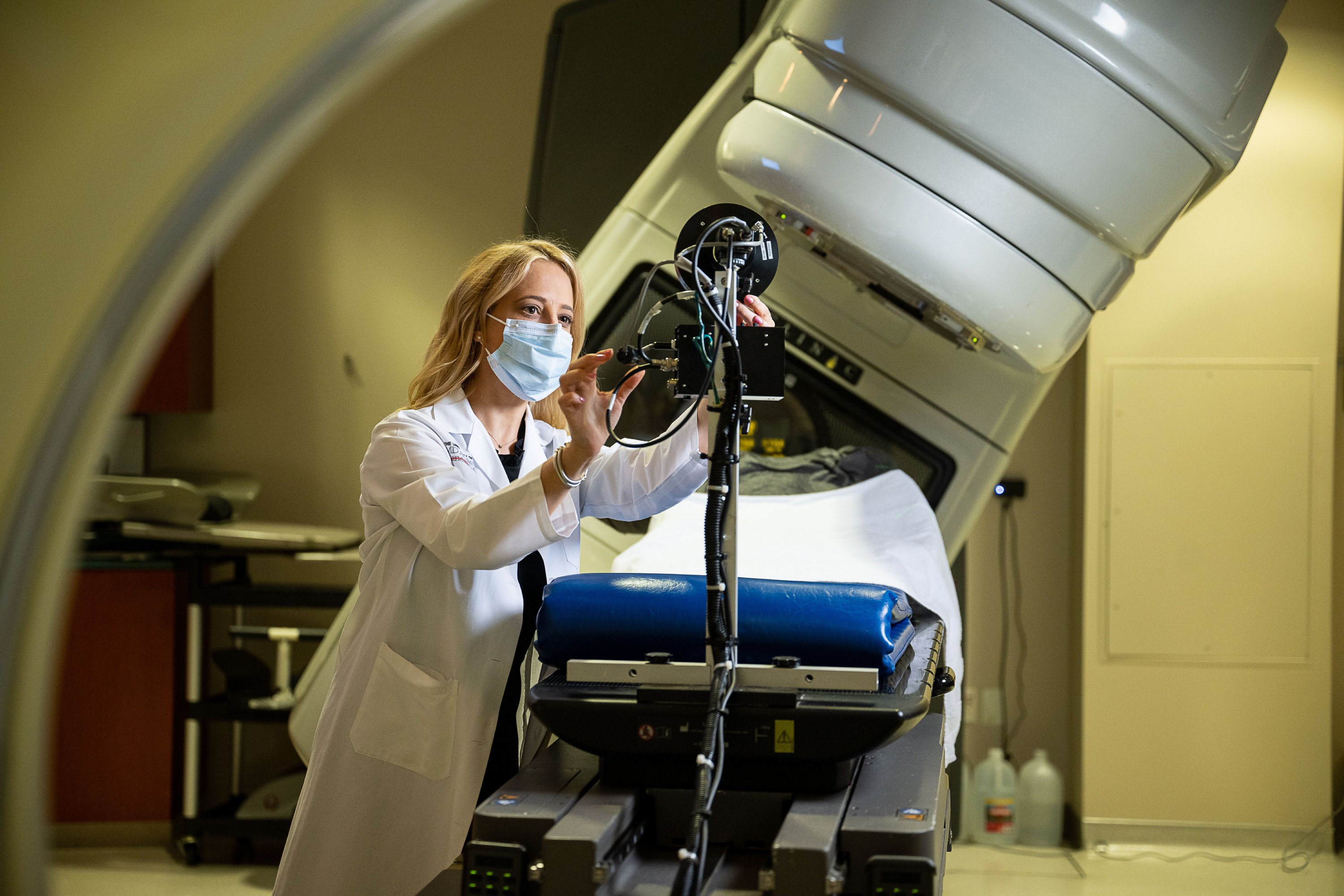
Side effects of radiation therapy for breast cancer
5 minute read | Published January 19, 2023
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on January 19, 2023
If you need radiation therapy as a part of your breast cancer treatment, you may have questions about side effects.
What are the most common side effects, for instance? How long will they last? And, is there any way to prevent or reduce them?
To learn more, we went to Wendy Woodward, M.D., Ph.D., a radiation oncologist and researcher who specializes in breast cancer.
What side effects does radiation therapy typically cause in breast cancer patients?
There are two “flavors” of side effects from radiation therapy, regardless of what type of cancer is being treated: early and late. The early side effects appear toward the end of treatment or within a few weeks of finishing it, while the late ones can appear anywhere from six months to a year after you’ve completed treatment.
The most common early side effects of radiation therapy in breast cancer patients are skin irritation and fatigue. Radiation therapy can last anywhere from one to six weeks. As you get farther into treatment, the skin on the breast or chest that’s repeatedly exposed to radiation can start to look dry or red and feel irritated. It may sometimes even peel.
When fatigue occurs, it usually appears toward the end of treatment. But many patients report that it’s mild or not as bad as the kind they experienced with chemotherapy.
What are the most common late radiation therapy side effects in breast cancer patients?
The skin of the breast or chest does not always go back to its normal color. So, there can be persistent tanning in the areas exposed to radiation. Daily moisturizing after you’ve finished treatment can help this fade. Radiation can also cause a tightening or hardening of soft tissues, so the exposed areas of the breast or chest wall might not feel as soft or as flexible as they once did. Stretching and physical therapy can be helpful to improve this. You may also notice little spider veins called telangiectasias, where the blood vessels have widened and become more visible under the skin’s surface.
Radiation therapy for breast cancer can slightly increase the risk of developing heart disease if the heart cannot be fully excluded from the treatment field. Exposing the heart to direct radiation can also cause acute pericarditis, which is inflammation of the sac-like structure surrounding the organ. But we really bend over backward to protect and avoid the heart during treatment at MD Anderson. So, I’ve never seen pericarditis from breast radiation even once in my 20 years here.
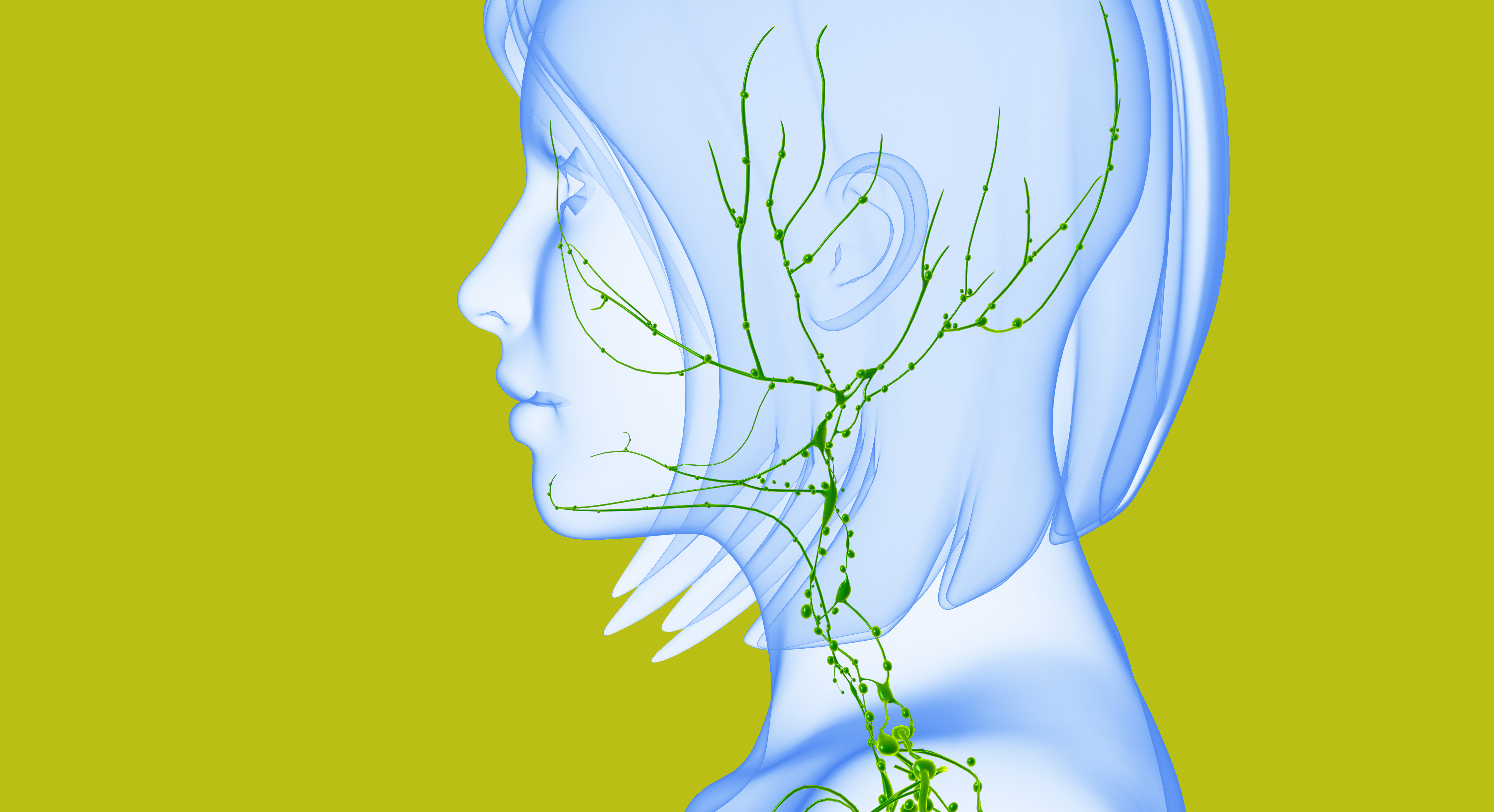
There’s also a risk of lymphedema, or swelling of the arm or upper body due to the inability of lymphatic fluid to drain properly. This happens sometimes when lymph nodes are removed from the neck, arm or torso. It can be more severe when the remaining lymph nodes are exposed to radiation. Lymphedema can be treated in many cases with surgery – either by surgically bypassing blocked lymph nodes or transferring new nodes into the affected areas.
There’s also a very low risk of developing a secondary cancer due to radiation exposure. But the benefits of getting rid of cancer now usually far outweigh the risks of a second diagnosis later.
How are these radiation therapy side effects treated?
For dryness and tenderness, we evaluate patients weekly. We want to see how their skin is holding up, so they don’t get too uncomfortable. If they start having issues, we can provide non-prescription lotions — or, at times, a topical steroid cream. There’s also a moisturizing gel product sold in sheet form that provides a cooling sensation when applied to the skin, and a number of foam dressings that are very helpful. For patients with skin pain, we recommend mixing a little topical lidocaine cream into their lotions to numb those areas while they heal.
For tightness and hardening, we usually recommend physical therapy. That can help patients regain their flexibility. For patients who choose to have breast reconstruction, our surgeons might replace some tissue in the affected areas with normal, non-irradiated tissue. Some patients have also found relief from pain and discomfort in tight muscles through Botox injections.
We also have clinical trials studying two topical steroids — mometasone and mepitel — to see if they can prevent skin reactions.
Pneumonitis, breast swelling, and other less common side effects
If patients have breast cancer that has spread to the lymph nodes in their necks, they may need radiation therapy to treat those nodes. This can cause a sore throat toward the end of treatment. It generally goes away on its own, but for patients who want immediate pain relief, we usually suggest ibuprofen or something similar.
Pneumonitis is another rare side effect. It may cause coughing or shortness of breath, and patients sometimes mistake it for the flu. It usually occurs between one and six months after finishing radiation therapy. It’s caused by irritation to the lung just under the ribs on the treated side of the body. Pneumonitis usually goes away on its own, but we can also treat it with steroids when needed.
Finally, some patients may experience swelling of the breast tissue. This generally goes away on its own and is fairly mild.
Is there any way to prevent skin-related radiation therapy side effects in breast cancer patients?
We plan our patients’ radiation therapy treatment very carefully to minimize “hot spots,” where particular patches of skin are exposed to higher doses of radiation than others.
Some studies suggest that topical steroids can prevent skin irritation, but it is not completely avoidable. When breast cancer involves the skin, we want to be sure the skin is adequately treated, so it gets a bit red as a result.
What new advances have been made to manage radiation side effects in breast cancer patients?
The Saphire clinical trial is studying whether side effects in breast cancer patients can be reduced by shortening the amount of time they receive radiation therapy.
The most exciting advance might be that we’ve found a mutation in the TGF-beta (transforming growth factor-beta) gene that appears to reveal a greater sensitivity to radiation therapy in some patients. Now, we’re trying to create a test to identify those patients before treatment begins so that we can make modifications to minimize their side effects.
Request an appointment at MD Anderson online or by calling 1-833-992-0260.

The early side effects appear toward the end of treatment or within weeks of finishing it.
Wendy Woodward, M.D., Ph.D.
Physician & Researcher