- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (66)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (68)
- Brain Metastases (28)
- Brain Tumor (230)
- Breast Cancer (718)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (152)
- Colon Cancer (164)
- Colorectal Cancer (110)
- Endocrine Tumor (4)
- Esophageal Cancer (42)
- Eye Cancer (36)
- Fallopian Tube Cancer (6)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (6)
- Kidney Cancer (124)
- Leukemia (344)
- Liver Cancer (50)
- Lung Cancer (288)
- Lymphoma (284)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (98)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (170)
- Pancreatic Cancer (164)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (144)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (236)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (60)
- Testicular Cancer (28)
- Throat Cancer (90)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (78)
- Vaginal Cancer (14)
- Vulvar Cancer (18)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (24)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (230)
- Epigenetics (6)
- Fertility (64)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (124)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (898)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (404)
- Survivorship (320)
- Symptoms (184)
- Treatment (1774)
Why managing heart health during and after cancer treatment is critical
4 minute read | Published August 09, 2018
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on August 09, 2018
Every year, the number of cancer survivors grows. That’s why it’s becoming increasingly important for doctors to make sure cancer treatments don’t cause any lingering side effects — particularly when it comes to heart health.
Heart problems are the leading cause of death in Americans each year. Cancer is No. 2. So if we’re able to cure someone’s cancer, we certainly don’t want to leave them with any cardiovascular issues.
Chemotherapy drug adversely affects heart function
Many cancer treatments can impair heart function. One is the chemotherapy drug doxorubicin, which is used frequently to treat breast cancer, as well as some sarcomas and lymphomas.
Doxorubicin has been around since the early 1970s and can reduce the heart’s ability to pump blood. Traditionally, this side effect has been described as “irreversible.” But we’re discovering that some of the patients we give heart-protective medication to show improvement, even years after they’ve completed treatment. So, that’s great news.
And, only about 2% of breast cancer patients will experience heart-related side effects from receiving the typical dose of doxorubicin. That goes up to about 5% in lymphoma and sarcoma patients, because of the higher doses used to treat those cancers.
Other treatments that affect heart function
Another drug that can affect the heart negatively is trastuzumab, which is a type of targeted therapy. Its effects have classically been described as “reversible.” That means if we stop administering the drug, the side effects disappear and the heart typically returns to normal within about four weeks. But even with newer targeted therapies, we are seeing less than 1% of patients have decreased-heart-function-related side effects.
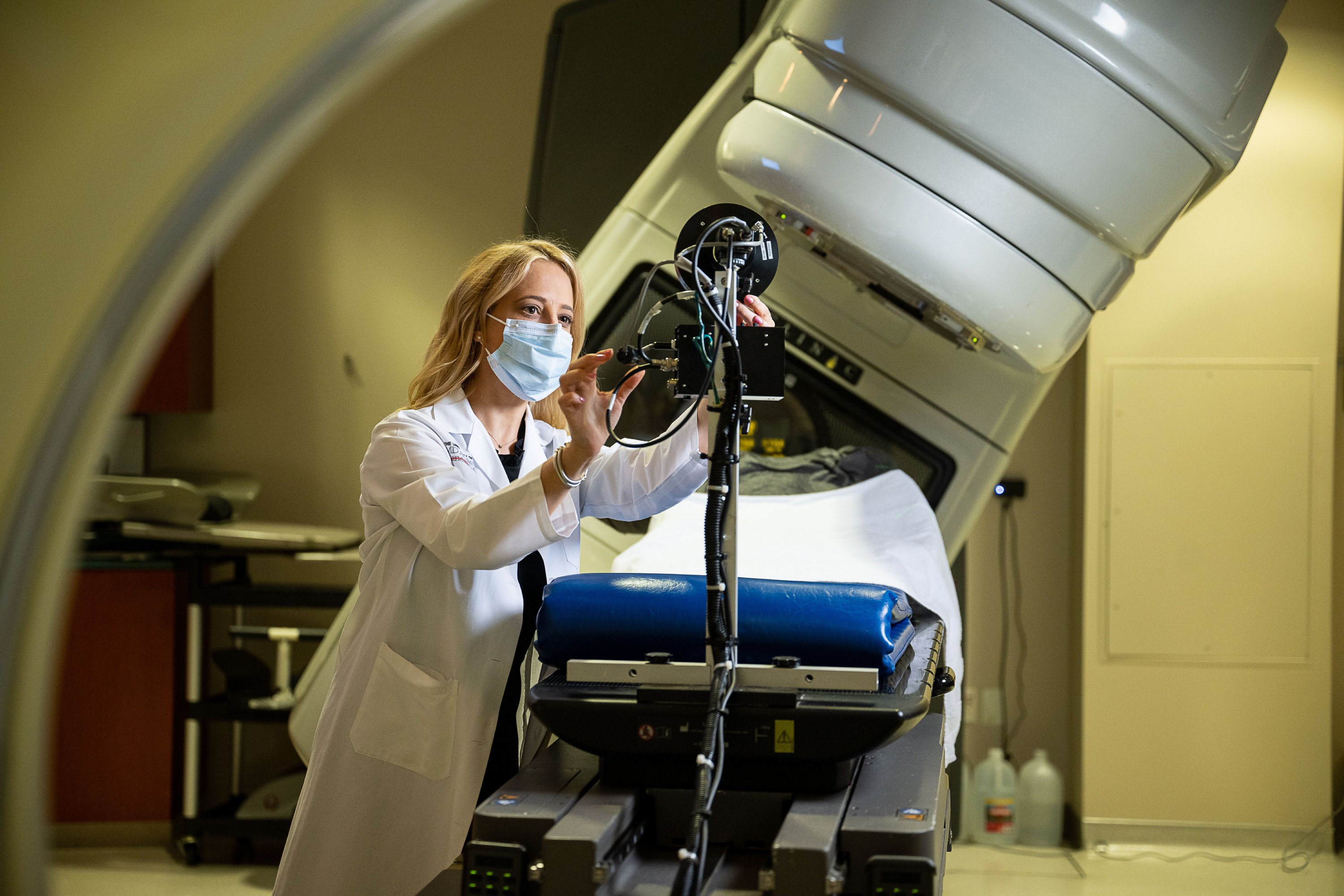
Radiation therapy has also been shown to cause heart blockages or valve problems, so patients being treated with radiation to the chest must be watched closely. MD Anderson has some of the best radiation oncologists around, and they are experts at limiting heart damage by focusing the radiation beams as much as possible on the cancer itself, instead of the surrounding tissues. But the heart is so close to some organs that it can still be affected.
Why getting a heart health baseline is so important
We don’t ever want to stop a patient’s cancer treatment prematurely. That’s why it’s critical for us to evaluate and test a patient’s heart function prior to starting any potential cardiotoxic treatment. This way, we can better recognize subtle signs of heart dysfunction as they occur and address them immediately.
We also want to keep watching patients even after they’ve finished treatment, as side effects can still show up 5, 10, 15 or even 20 years down road.
Managing other risk factors
Keep in mind that heart damage stemming from cancer treatment is still pretty rare. In fact, only about 5% of my cardiology patients have heart problems related to cancer treatment. The rest had heart problems prior to treatment, or developed completely unrelated heart issues later on.
There are a lot of other risk factors that can damage the heart, too — such as hypertension, diabetes, and high cholesterol. That’s why I tend to look for the more common causes of problems, like clogged arteries or heart attacks, and rule those out first.
Symptoms of heart failure to look for
At MD Anderson, our cardiologists use ultrasounds, EKGs and other tests to monitor heart function. But there are some signs of heart failure or blockages that patients can look for. These include:
- Chest pain or pressure, especially when you’re exerting yourself, such as taking the stairs or gardening
- Feeling more out of breath than usual (e.g., noticing you have to take a break and rest, even while grocery shopping)
- Swelling in the legs (e.g., your socks make indentations on both feet, which can signal fluid build-up in the body because the heart is not pumping adequately)
- Sleeping at an angle (because you’re short of breath when you lie flat in bed)
We tell patients to call immediately if they start seeing any of these symptoms. When they do, we perform an ultrasound and/or other tests to determine if it’s their heart. Often, these symptoms can be managed with diuretics, which help the body shed excess fluid, and other cardiac medications.
What patients can do to protect their heart health
To minimize the risk of heart damage from cancer treatments, we recommend that you:
- Stay active. The American Institute for Cancer Research and the American College of Sports Medicine recommend 150 minutes of moderate physical activity or 75 minutes of vigorous exercise each week. Maintain your ability to climb a flight of stairs or swim laps in a pool.
- Maintain a healthy weight. If you’re overweight, losing just 5-10% of your body weight has huge health benefits.
- Follow a Mediterranean-style or mostly plant-based diet that is limited in sugar.
Remember, most patients are unlikely to develop heart problems caused by cancer treatments, but all of these things will serve you well, if you do.
Nicolas Palaskas, M.D., is a cardiologist at MD Anderson. Dr. Palaskas will be sharing more insight on cardiac monitoring during and after treatment at this year’s myCancerConnection Cancer Survivorship Conference. Register to attend on Sept. 13 and 14.
Request an appointment at MD Anderson online or by calling 1-888-695-3090.

Heart damage stemming from cancer treatment is still pretty rare.
Nicolas Palaskas, M.D.
Physician