- Diseases
- Acoustic Neuroma (16)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (18)
- Bile Duct Cancer (26)
- Bladder Cancer (74)
- Brain Metastases (28)
- Brain Tumor (234)
- Breast Cancer (728)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (168)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (130)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (178)
- Pancreatic Cancer (162)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (150)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (302)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (100)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (22)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (240)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (122)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (940)
- Research (390)
- Second Opinion (78)
- Sexuality (16)
- Side Effects (616)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (408)
- Survivorship (330)
- Symptoms (182)
- Treatment (1794)
Nanomedicine: Small particles with huge possibilities for cancer care
4 minute read | Published February 10, 2021
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on February 10, 2021
Nanomedicine is a quickly emerging area of study that uses nanoparticles for drug delivery, diagnoses and in vivo imaging. While nanomedicine may sound like science fiction, MD Anderson researchers are studying it to better understand how it can be used to improve cancer treatment. In fact, MD Anderson is one of the few centers in the country leading research in this field.
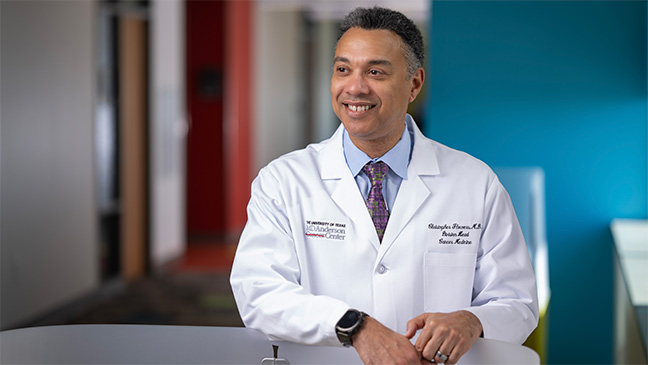
Here, Betty Kim, M.D., Ph.D., associate professor of Neurosurgery, talks about the progress being made in nanomedicine and its potential use in cancer care. Kim recently published a perspective paper on nanomedicine in Nature Nanotechnology.
What is nanomedicine?
Nanomedicine is defined as materials that are within 1 to 100 nanometers in size that, ultimately, should be able to specifically target tumor cells or immune cells of interest. It can also have a multiplexing capability. It can be used for imaging, diagnostics and therapeutics and other applications as well.
Researchers are exploring use of nanomedicine for immunotherapy. What makes it such a powerful platform for immunotherapy?
When it comes to how we use this for immunotherapy, that's actually a new area. This is the next frontier of designing drugs.
The goal of chemotherapy is to kill the cancer by giving the patient as much of the drug as possible. As a result, the whole body receives this massive dose of drugs, which causes hair loss, diarrhea and nausea. However, nanomedicine provides a strategy to deliver anti-cancer or immunotherapy drugs in a more targeted manner, while avoiding the healthy tissues. As a result, we’re able to minimize a lot of those side effects.
Nanomaterials can be designed to interact with the body’s immune system either to boost its function, as in the case against cancer, or dampen it, as when there is potential risk of autoimmune reactions.
Think of nanomaterials as a LEGO® set. You can choose individual pieces to build a complex machine that can perform a specific function. Nanoengineering is similar: you pick the starting material, whether is a lipid or polymer, and design medicine in a way that can perform tasks such as activate immune cells.
In your paper, you outline key variables that impact immune nanomedicine research: the microbiome, sex, age, environment, immunotherapy and toxicity responses. Why is it so important for scientists to make these distinctions when designing these types of clinical trials?
There's been a lot of buzz over nanomedicine over the past 20 years, but unfortunately, there haven’t been many breakthroughs. We're realizing that it's very complex to create these materials. Now that we have immunotherapy, which has really changed the way we treat cancer, it adds another layer of complexity. Since we’re now targeting the immune cells, we have to understand the patient better.
With immunotherapy, we know the microbiome, sex, age, environment and the body’s responses to immunotherapy and toxicity affect the immune system, so all of those things need to be taken into consideration when designing clinical studies.
What major success has there been in the field of nanomedicine so far?
Both the Moderna and Pfizer-BioNTech’s COVID-19 vaccines use lipid-based nanoparticles to fight the SARS-CoV-2 virus.
These two vaccines use mRNA to transcribe viral proteins that the body’s immune system can recognize and use to develop immune memory. However, when injected into the body, mRNA itself is rapidly degraded. It can’t get to the intended targets on its own, which in this case, are the immune cells. Therefore, it requires a delivery vehicle.
This is where nanotechnology comes in: the mRNA is encapsulated within lipid nanoparticles that helps shuttle it to the designated organ and tissue of interest.
Tell us about the nanomedicine work your lab is doing.
We're working on utilizing nanomaterials as active – not as passive – compounds. Traditionally, you inject the genetic material and assume it'll somehow get to the tissue where it will then engage with the tumor cells. However, we’re working on developing what’s called an engager system. This system uses nanoparticles coated with two components to deliver a one-two punch to shrink tumors: antibodies that target the HER2 receptor and calreticulin molecules that interact with the immune cells. Essentially, the nanoparticles are designed to act like heat-seeking missiles: the antibodies allow the nanoparticles to seek cancer cells, while the molecules engage the immune system’s macrophages and phagocytes destroy them. After the macrophages eat up the cancer cells and chop them up into little fragments, they’re presented on the surface of the macrophages.
T cells then recognize these cancer cell fragments, called peptides, and reprogram them to attack the other cancer cells. What’s really cool about this is that a portion of T cells become memory T cells, so once you have that event, it can prevent other types of tumors within that family from growing.
We are currently working on expanding the same concept to other molecules and cancers in my lab.
How will nanomedicine benefit cancer patients in the future?
For some types of cancer, like glioblastoma and triple-negative breast cancer, patients really only have one treatment option. Our lab would like to change that. In cancer, nanomedicine can be used to boost immune response against tumors by serving as an adjuvant for vaccine therapy or as drug carriers that can help us target tumors more effectively with anti-cancer agents, while leaving normal tissues untouched.
Refer a patient to MD Anderson online or by calling 1-833-569-1784.
Related Cancerwise Stories

Nanomaterials can be designed to interact with the body’s immune system either to boost its function, as in the case against cancer, or dampen it, as when there is potential risk of autoimmune reactions.
Betty Kim, M.D., Ph.D.
Physician & Researcher