- Diseases
- Acoustic Neuroma (16)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (18)
- Bile Duct Cancer (26)
- Bladder Cancer (74)
- Brain Metastases (28)
- Brain Tumor (234)
- Breast Cancer (728)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (168)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (130)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (178)
- Pancreatic Cancer (162)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (150)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (302)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (100)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (22)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (240)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (122)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (940)
- Research (390)
- Second Opinion (78)
- Sexuality (16)
- Side Effects (616)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (408)
- Survivorship (330)
- Symptoms (182)
- Treatment (1794)
Molecular profiling gives pancreatic cancer survivor more options
5 minute read | Published April 28, 2021
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on April 28, 2021
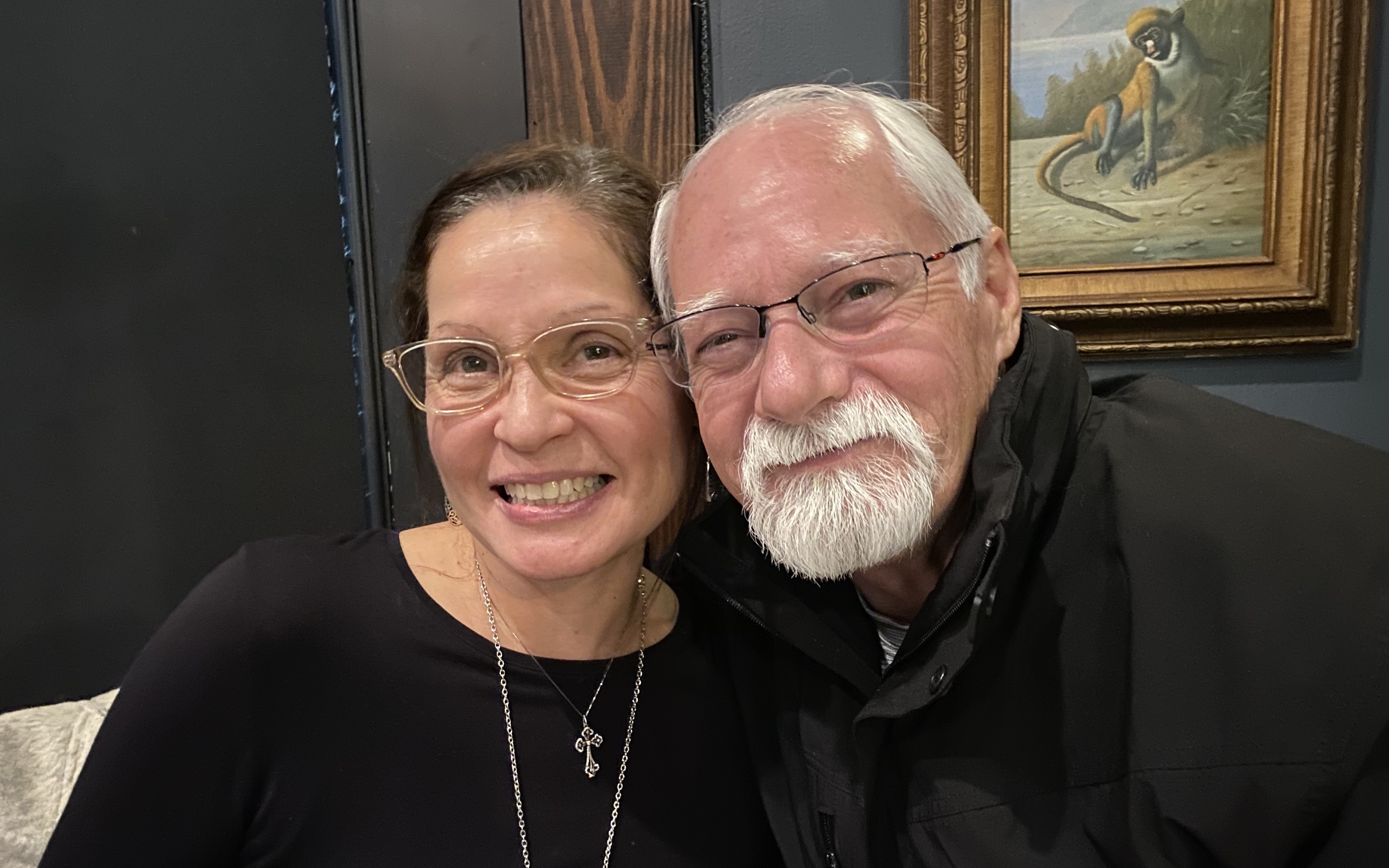
Drew Huggins still gets emotional when he recalls the day clinical trial coordinator Jing Yang phoned him with some good news that changed the course of his pancreatic cancer treatment.
“My two brothers were driving me to my physical therapy appointment,” he says, “because I was too weak to drive myself.”
Yang told Drew about a new experimental drug that was being tested at MD Anderson through a clinical trial. Unlike previous treatments that had failed to control the pancreatic cancer, this drug was designed to target the exact genetic mutation that caused his cancer to grow.
“That phone call gave me hope,” Drew recalls.
A pancreatic cancer diagnosis
Drew’s first signs of trouble began two years ago, with chest pains and a dull ache in his stomach that radiated to his back.
An MRI in his hometown of San Antonio revealed the source of his discomfort: an egg-sized cancerous tumor inside Drew’s pancreas. It was aggressive, and it had spread to his liver.
“The doctor explained that the tumor was pressing on my spine, which caused the pain in my back,” Drew says. “And my chest pain was caused by three tumors that had spread from my pancreas to my liver.”
The doctor advised following up with a local oncology group, but Drew called MD Anderson instead.
“MD Anderson is the top-rated cancer center in the nation, and it’s only three hours from my home,” he says. “Why would I consider going anywhere else?”
Side effects of pancreatic cancer treatment
At MD Anderson, medical oncologist Janet Tu, M.D., placed Drew on FOLFIRINOX, a combination of four chemotherapy drugs used to treat pancreatic cancer that has spread to other parts of the body. He was supposed to undergo 18 cycles, but the intravenous infusions were discontinued after only 13 cycles when an MRI showed the treatment didn’t work.
Drew was then given the chemotherapy drugs gemcitabline and paclitaxel, but those didn’t work, either. Not only was the cancer still spreading, but the drugs were causing weakness, numbness and pain in his hands and feet. After only four cycles of an 18-cycle regimen, the treatment was discontinued.
It was time to try something new. Gastrointestinal medical oncologist Shubham Pant, M.D., enrolled Drew in a clinical trial that was testing an experimental antibody drug conjugate, or ADC – a highly potent drug built by attaching an anticancer drug to a disease-fighting antibody. Like a guided missile, the antibody zeros in on the tumor, then releases its payload of toxic drugs to kill the cancer cells.
But the therapy didn’t work for Drew. In fact, his tumor grew by 25%.
A targeted drug for pancreatic cancer
Drew was quickly running out of options when Pant suggested sending tissue from his tumor to a lab for genetic testing – a practice known as comprehensive tumor profiling. If the test uncovered a genetic mutation that caused Drew’s cancer, he could then be matched with a cancer drug that targeted his specific mutation.
“Only a small percentage of all pancreatic cancer patients have mutations that can be targeted,” Pant warned. “But if we don’t look for a mutation, we’ll never find it. It’s worth a try.”
Luck was on Drew’s side. The test revealed that his tumor harbored a rare NRG1 fusion, which occurs when the NRG1 gene fuses with another unrelated gene. People with a NRG1 fusion produce too much of the growth factor neuregulin1 (NRG1), which can cause cancer cells to grow out of control.
A mere 1.5% of all pancreatic cancers contain NRG1 fusions, and Drew was one of them. This meant he could enroll in a clinical trial at MD Anderson, where a drug named zenocutuzumab (also called MCLA-128) is being tested in patients with NRG1-induced cancer.
Last July, the Food and Drug Administration granted zenocutuzumab “orphan” status for the treatment of pancreatic cancer. Orphan drugs are those that treat rare diseases that affect less than 200,000 people in the U.S. And because there is no approved therapy to treat tumors caused by NRG1 fusions, the FDA this January granted the drug fast-track designation, meaning it will go through a quicker review and approval process to fill an unmet medical need.
Tailoring treatment to each pancreatic cancer patient
“Every patient’s pancreatic cancer is different,” says Jordi Rodon Ahnert, M.D., Ph.D., who specializes in early drug development and precision medicine. He heads the MD Anderson arm of the international eNRGy clinical trial that's testing zenocutuzumab – the trial Drew joined.
“A one-size-fits-all approach won’t work,” Rodon Ahnert says, “because two people can have pancreatic tumors that genetically look nothing alike. Molecular profiling that sequences a tumor's DNA and RNA can help us tailor the best treatment to each unique individual.”
The American Society of Clinical Oncology reinforced this approach last year by issuing new guidelines that call for all pancreatic cancer patients who are likely to benefit from treatment after chemotherapy to undergo molecular profiling.
“Targeted therapy offers much hope to patients with NRG1 fusion-positive tumors by aligning their treatment with their biology,” says Pant, who contributed to the new guidelines.
A personalized medicine approach to pancreatic cancer treatment
Since starting the trial last September, Drew has been steadily getting stronger. He’s gained weight, his pain has significantly lessened, and he’s more active.
Today, his tumors have shrunk dramatically. His tests and scans show no tumor activity, and he no longer has to deal with the side effects caused by other treatments.
A recent laboratory test showed that Drew’s number of CA 19-9 molecules, which are released by pancreatic cancer cells, has decreased by 90% since he enrolled in the trial.
“Every time I go for a checkup, the news just gets better,” he says.
Drew’s progress is so remarkable that he is now enrolled in the Unusual Responders Program in MD Anderson's Institute for Personalized Cancer Therapy. In this program, participants who respond exceptionally well to therapy donate their tissue samples for scientific study.
“As clinicians and researchers, we have much to learn from these patients,” Pant says. “The knowledge we gain will help shift cancer treatment away from conventional therapies and toward a more personalized medicine approach.”
Request an appointment at MD Anderson online or by calling 1-866-403-3911.
Related Cancerwise Stories

Two people can have pancreatic tumors that genetically look nothing alike.
Jordi Rodon Ahnert, M.D., Ph.D.
Physician & Researcher