- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (66)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (28)
- Bladder Cancer (68)
- Brain Metastases (28)
- Brain Tumor (230)
- Breast Cancer (716)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (154)
- Colon Cancer (164)
- Colorectal Cancer (110)
- Endocrine Tumor (4)
- Esophageal Cancer (42)
- Eye Cancer (36)
- Fallopian Tube Cancer (6)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (6)
- Kidney Cancer (124)
- Leukemia (344)
- Liver Cancer (50)
- Lung Cancer (288)
- Lymphoma (284)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (98)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (170)
- Pancreatic Cancer (166)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (144)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (236)
- Skin Cancer (294)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (60)
- Testicular Cancer (28)
- Throat Cancer (90)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (78)
- Vaginal Cancer (14)
- Vulvar Cancer (18)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (624)
- Complementary Integrative Medicine (24)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (230)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (122)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (892)
- Research (390)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (404)
- Survivorship (322)
- Symptoms (184)
- Treatment (1772)
Dysphagia in cancer patients: What to know
6 minute read | Published August 05, 2019
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on August 05, 2019
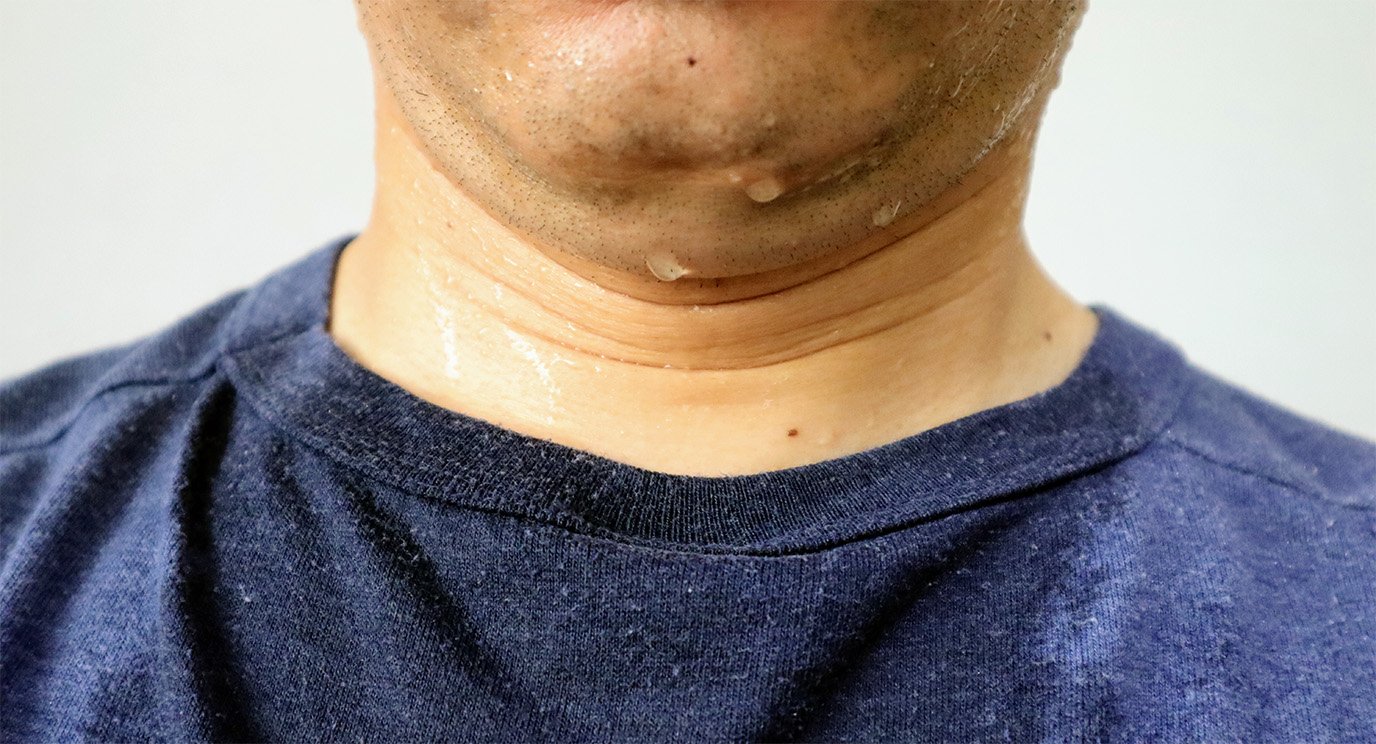
The ability to swallow — or to eat and drink what you enjoy most without choking or coughing — is something that many of us take for granted. And most people never think about how they eat or drink until they experience dysphagia, or trouble swallowing.
Cancers in the mouth, throat or esophagus can make it difficult to swallow. If the ability to swallow is compromised because of a cancer diagnosis or its treatment, it can get better after treatment is finished. Unfortunately, that is not always the case.
Here are answers to some of the questions I hear most often from patients with dysphagia — and what doctors at MD Anderson are doing to prevent and treat it.
What is dysphagia and why do I have it?
Dysphagia is the medical term for “having trouble swallowing.” In cancer patients, it can be caused by the tumor itself (usually in head and neck cancers) — which blocks or narrows the food passage — or as a side effect of treatment.
A tumor in the head or neck can interfere with the ability of the lips, tongue, or throat muscles to move food around the mouth so that it can be chewed and passed to the esophagus. In other cases, the tumor may block the throat so that food and/or liquid cannot pass through it.
Radiation therapy can also cause swallowing problems. The effects of radiation — including scarring and fibrosis — build over time, and can reduce the ability of the throat muscles to function properly, even long after treatment is finished. Radiation can also cause narrowing of the swallowing passage — a problem known as "stricture."
Chemotherapy doesn’t generally cause lasting dysphagia, but it can make the effects of radiation worse. And though chemotherapy can also affect a patient’s appetite and desire to eat, those side effects are often temporary. The side effects of radiation are usually permanent.
Surgery can cause swallowing problems by removing structures in the head, neck or esophagus that normally allow food and liquids to pass through the system.
How is dysphagia diagnosed?
If you report trouble swallowing, your doctor will order tests to watch the food and water pass through your mouth and throat as you eat and drink. These tests may use imaging (such as X-rays during a modified barium swallow study) or a flexible scope to look inside your throat.
The degree of your dysphagia will be rated on both the efficiency and the safety of your swallows.
Swallowing efficiency is how quickly and effortlessly you’re able to swallow. “Inefficient” swallowing results in food being left behind in the mouth or throat. It might take a long time for you to eat, or feel like something’s been “left over” or “stuck” in your throat after each bite.
Swallowing safety is the ability to eat and drink without anything entering the airway, also known as “aspiration.” Food and liquid that enter your airway can cause pneumonia. So, it’s important to undergo a swallowing examination that evaluates your ability to protect the airway.
Swallowing difficulties in the mouth and throat are called "oropharyngeal dysphagia" and are evaluated and managed by speech-language pathologists in the Head & Neck Center. Swallowing difficulties in the esophagus are called "esophageal dysphagia" and are evaluated and managed by specialists in the Gastroenterology Center.
How might dysphagia affect my ability to eat?
Certain types of food, such as solids or those with grainy textures, may be harder for you to swallow than others. This can limit your diet. Some patients find that drinking liquid supplements — such as shakes and smoothies — helps them maintain their weight when swallowing is difficult. In other cases, you may need a feeding tube to ensure you’re receiving adequate nutrition while you heal.
In situations where swallowing a pill becomes impossible, ask your doctor to prescribe a liquid version of the medication, if it’s available. Or, ask your pharmacist if your medications can be crushed.
Do you have any special dietary recommendations for me?
No, because not everyone with dysphagia can eat the same foods. It is crucial to receive proper guidance regarding the types of foods and liquids that are safe for you to swallow.
These recommendations should come from a speech-language pathologist with experience working with cancer patients. A knowledgeable dietitian can provide information on how to make sure your diet is meeting your nutritional needs.
If you’re an MD Anderson patient, you can ask a member of your care team for a referral to one of our dietitians or speech-language pathologists.
When should I approach my doctor for help with dysphagia?
Ideally, you would meet with a speech-language pathologist who has experience working with cancer patients before starting treatment, so that you could receive the appropriate testing, counseling and information needed to prevent or lessen the severity of dysphagia.
Once you’re actually having problems swallowing, you can still seek help. However, in general, the earlier therapy starts, the better the outcome. Some aspects of the dysphagia may be irreversible.
How will my dysphagia be treated?
Dysphagia can be treated using a variety of methods, including exercises, postures (such as head turns or chin tucks), massage techniques and muscle manipulation. In some cases, a gastroenterologist may need to stretch or dilate a tight area of your throat or esophagus under sedation, to allow food to pass through more easily.
Are my cancer-related swallowing issues temporary or permanent?
They can be either. It depends on the type of tumor, the size of the tumor, the stage of your disease and the type of treatment you’re getting. All of these factors play a role in determining the severity of dysphagia and your ability to recover from it.
That’s why it is critical to meet with an experienced speech-language pathologist before cancer treatment begins. This ensures you’ll get the guidance needed to preserve as much swallowing function as possible.
What are the latest advances in dysphagia treatment?
One advancement we're currently studying is releasing muscles that have become “frozen,” so that they can move freely again, and then strengthening them so that patients can eat and drink efficiently and safely.
New rehabilitative treatments are also helping some long-term cancer survivors regain their ability to swallow, so they can take at least some food by mouth (rather than relying exclusively on tube feeding).
Is there anything new and exciting on the horizon?
From a prevention standpoint, we’re studying the most effective (and least burdensome) ways that patients can maintain their swallowing muscles during treatment.
We’re also partnering with surgeons and radiation oncologists to explore better ways of maintaining swallowing function, such as by reducing the amount of radiation delivered to areas without cancer. And we’re investigating new surgical techniques to avoid injuring muscles that are critical to swallowing. This includes methods using robotic and laser technology. The results have been positive so far. In some cases, patients have been able to avoid radiation therapy entirely.
Finally, we’re conducting new swallowing rehabilitation studies to determine the specific types of exercises and frequency needed to make a difference for our patients.
What’s the one thing I should know about dysphagia?
The enemy of swallowing is NOT swallowing, so strive to preserve as much function as possible. Our philosophy is "use it or lose it." Keep those muscles moving, whether the goal is to maintain normal function going into your cancer treatment or to restore function that has been lost during the process.
Kate Hutcheson, Ph.D., is an associate professor in Head and Neck Surgery, and Chief of Speech Pathology and Audiology at MD Anderson.
Request an appointment at MD Anderson online or by calling 1-855-781-4421.
Related Cancerwise Stories

Keep those muscles moving.
Kate Hutcheson, Ph.D.
Chief, Speech Pathology and Audiology