- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (66)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (28)
- Bladder Cancer (68)
- Brain Metastases (28)
- Brain Tumor (230)
- Breast Cancer (718)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (154)
- Colon Cancer (164)
- Colorectal Cancer (110)
- Endocrine Tumor (4)
- Esophageal Cancer (42)
- Eye Cancer (36)
- Fallopian Tube Cancer (6)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (6)
- Kidney Cancer (124)
- Leukemia (344)
- Liver Cancer (50)
- Lung Cancer (288)
- Lymphoma (284)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (98)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (170)
- Pancreatic Cancer (166)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (144)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (236)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (60)
- Testicular Cancer (28)
- Throat Cancer (90)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (78)
- Vaginal Cancer (14)
- Vulvar Cancer (18)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (626)
- Complementary Integrative Medicine (24)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (230)
- Epigenetics (6)
- Fertility (64)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (124)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (896)
- Research (390)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (404)
- Survivorship (322)
- Symptoms (184)
- Treatment (1776)
Can a pregnancy test predict testicular cancer?
4 minute read | Published March 22, 2021
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on March 22, 2021
A social media post about a man’s positive pregnancy test reportedly led to his testicular cancer diagnosis.
The man jokingly took the test which an ex-girlfriend had left behind in his medicine cabinet. He shared the surprising “positive” result with a friend, who shared the news on social media, carefully shielding the test-taker’s name to protect his privacy. The post quickly went viral and drew more than 1,600 comments.
“If this is true, you should check yourself for testicular cancer. Seriously. Google it,” read one of the comments.
A trip to the doctor revealed the male pregnancy-test-taker did, in fact, have testicular cancer.
Not all testicular cancers are alike
Pregnancy tests work by detecting human chorionic gonadotropin (HCG), a hormone in the blood and urine produced by the developing placenta.
It turns out that some types of testicular cancer make the same hormone.
So, is it worth running out to buy a pregnancy test to check for testicular cancer?
“There’s no advantage to relying on a pregnancy test to self-diagnose testicular cancer. It’s even dangerous to do so,” says urologist Christopher Wood, M.D. “Some forms of testicular cancer cause elevated HCG levels, but others don’t. Someone could get false reassurance from a negative test or could have elevated HCG levels for another reason altogether.”
Instead, Wood says men should see a doctor if they notice testicular cancer symptoms or unusual changes, including a lump or enlargement in either testicle, a sensation of heaviness in the scrotum, or a sharp pain or discomfort in the scrotum or testicle.
He recommends performing a self-exam in the shower once a month, starting in puberty.
“Testicular cancer manifests itself most commonly as a painless scrotal mass,” Wood says, “so check yourself, know your body and see a doctor if you detect anything suspicious.”
Testicular cancer risk factors
Compared to other types of cancer, testicular cancer is rare, accounting for just 1% of all cancers that occur in men. Yet it’s the most common cancer in males ages 15 to 35.
“This is a disease of the young,” Wood explains. “The typical patient is in his 20s or 30s, though we’ve seen patients as young as 15 and as old as 55.”
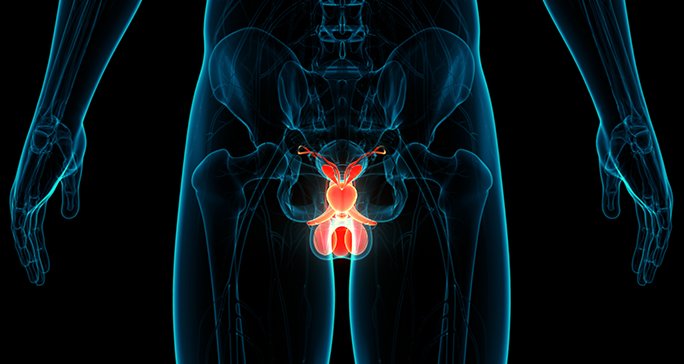
The disease occurs when cells in the testicles grow and multiply out of control, causing tissue damage and disrupting the normal function of the testicle.
The exact causes of testicular cancer are unknown, but a number of factors have been identified that increase a man’s risk of developing the disease, including undescended testicles at birth, a family history of testicular cancer, or a previous testicular cancer diagnosis.
How is testicular cancer diagnosed?
A scrotal ultrasound is usually the first step in diagnosing testicular cancer. It’s a painless procedure that gives a clear indication of whether a mass in the testicle is solid or filled with fluid. A fluid-filled lump is usually harmless. A more solid lump may signal that the swelling is cancerous.
The next step is a blood test. Many testicular cancers make high levels of certain proteins called tumor markers such as HCG and alpha-fetoprotein (AFP), which are both associated with pregnancy. When these tumor markers are in the blood, it suggests that there's a testicular tumor.
Rises in levels of HCG or AFP can also help doctors tell which type of testicular cancer it might be.
A testicular tumor might also increase the levels of an enzyme called lactate dehydrogenase (LDH). A high LDH level often, but not always, indicates widespread disease. But, LDH levels can also be increased with some non-cancerous conditions.
How is testicular cancer treated?
The first treatment for all cases of testicular cancer, whatever the stage, is an orchidectomy – a surgical procedure to remove the testicle.
“By removing the entire affected testicle, your chances of making a full recovery are greatly improved,” Wood explains. “Removing only the tumor may result in the cancer spreading.”
Sex life and the ability to father children are typically not affected, he says.
After surgery, doctors monitor HCG level to determine if the cancer is gone.
“If the patient had elevated levels of HCG before surgery, you would expect those level to return to normal after surgery,” Wood says. “If they don’t, it means there are residual cancer cells that have to be treated with chemotherapy or radiation.”
Testicular cancer survival rates
Testicular cancer is highly treatable, even when cancer has spread beyond the testicle.
“While a cancer diagnosis is always serious,” Wood says, “the good news about testicular cancer is that the vast majority of cases – even if they're caught further along – are still very curable.”
Request an appointment at MD Anderson online or by calling 1-833-903-3675.

Someone could get false reassurance from a negative test.
Christopher Wood, M.D.
Physician