- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (294)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (96)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (630)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (912)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (320)
- Symptoms (182)
- Treatment (1786)
Bugs as drugs: What is microbial cell therapy?
3 minute read | Published November 05, 2024
Medically Reviewed | Last reviewed by Christopher Johnston, Ph.D., on November 05, 2024
When it comes to cancer therapies, the use of bacteria may sound unusual, but it’s a rapidly developing field with exciting potential.
Genomic medicine researcher Christopher Johnston, Ph.D., and his team are developing microbial cell therapies. That is, they are gearing up to use bacteria to target and treat cancer directly.
"Using ‘bugs as drugs’ offers a promising solution to overcome some of the challenges with traditional cancer therapies," says Johnston. "Solid tumors, which account for the majority of adult cancers, can be notoriously treatment-resistant due to their complex microenvironment. But harnessing the unique abilities of certain microbes may give us a new way to tackle those barriers.”
How microbial cellular therapies work
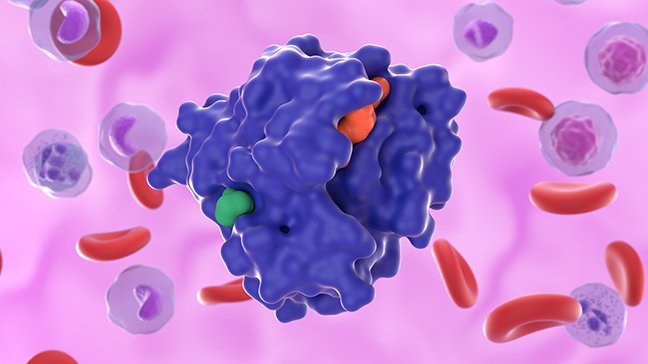
Microbial cell therapies aim to use engineered bacteria to attack cancer cells directly or to assist standard therapies, such as chemotherapy and immunotherapy, by delivering therapeutic agents directly within the tumor microenvironment.
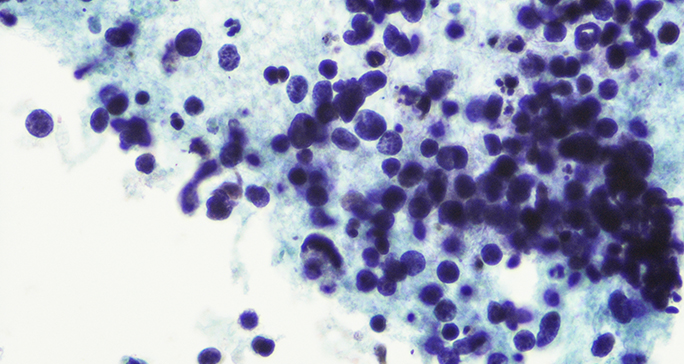
Several types of bacteria, including Listeria, Salmonella, Escherichia (E. coli) are being studied as potential platforms for these therapies. These bacteria are first grown in the lab and then re-engineered to produce cytotoxic (cell-killing) or immunostimulatory molecules that help break down the tumor cells or stimulate a desired ‘anti-tumor’ immune response.
This targeted approach could improve treatment efficacy while also minimizing damage to healthy tissues, explains Johnston. “Think of the engineering of microbes as tiny, programmable robots that could be enhanced in their tumor targeting abilities to deliver therapeutic agents directly where they’re needed most,” he says.
Harnessing the power of microbes for good
To overcome some of the challenges faced by early microbial cell therapies, researchers are now exploring a "reverse translation" approach, harnessing bacteria that have already shown the ability to naturally infiltrate human tumors, especially along the gastrointestinal (GI) tract.
Johnston, along with immunology researcher Susan Bullman, Ph.D., found that one such bacterium, Fusobacterium nucleatum (Fn), has shown promise in this area.
Fn is a microbe typically found in the mouth; it has also been found at high levels in colorectal cancer tumors, as well as in oral, esophageal and pancreatic cancers. The presence of this bacteria in colorectal cancer patients’ tumors has been linked to cancer recurrence, metastasis and an overall poorer prognosis.
But there is one subspecies of Fn that Johnston and Bullman are most interested in: Fna C2.
Rarely found in the healthy gut, Fna C2 thrives in the same part of the CRC tumors that are hardest to treat with traditional therapies: regions with low oxygen levels and poor blood flow, which are also highly immunosuppressive. These areas are often resistant to immune-based treatments like CAR T cell therapy.
Bullman says that leveraging Fna C2’s natural ability to target tumors, while “stripping away” the parts that make the pathogen harmful, could make bacterial therapies a powerful complement to existing treatments or even serve as a stand-alone option for some patients.
The future of microbial cell therapies
There are risks of leveraging the natural behavior of these bacteria in hopes of creating new cancer treatments. Cancer patients are often immunocompromised, so introducing bacteria could raise their risk of infection.
This is why Johnston says strict containment strategies and “kill-switches” are necessary.
“It is crucial to maintain precise control over these microbes, ensuring they can selectively target specific areas in the body, deliver therapeutic payloads and then cease all activity,” he explains.
Researchers in the Johnston Lab are engineering the bacteria with dependencies, such as genetic circuits that ensure the bacterial cells burst open and die once they have completed their jobs. Targeted antibiotics are another possible method of control.
While microbial cell therapies using Fna C2 are still in the early stages, Johnston sees potential in the bugs’ abilities to target hard-to-reach tumor regions and deliver therapies directly.
“In colorectal cancers, we see these bacteria in the tumor microenvironment of roughly half of the tumors analyzed,” Johnston says. “If we can exploit this existing relationship for microbial cell therapies, it may give cancer patients another treatment option, targeting cancer from the inside out.”
Johnston will be speaking about Microbial Cell Therapies: Challenges and Opportunities for Bugs as Drugs at the Society for Immunotherapy of Cancer in Houston on Friday, Nov. 8.
Learn about research careers at MD Anderson.

Think of the engineering of microbes as tiny, programmable robots that could be enhanced in their tumor targeting abilities to deliver therapeutic agents directly where they’re needed most.
Christopher Johnston, Ph.D.
Researcher