- Diseases
- Acoustic Neuroma (16)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (18)
- Bile Duct Cancer (26)
- Bladder Cancer (74)
- Brain Metastases (28)
- Brain Tumor (234)
- Breast Cancer (726)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
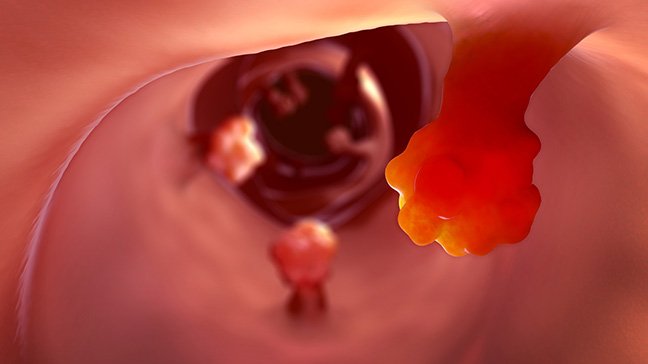
- Colon Cancer (168)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (130)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (178)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (150)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (300)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (100)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (22)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (238)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (122)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (936)
- Research (390)
- Second Opinion (78)
- Sexuality (16)
- Side Effects (616)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (408)
- Survivorship (328)
- Symptoms (182)
- Treatment (1788)
Asbestos exposure and cancer: 8 things to know
4 minute read | Published January 27, 2025
Medically Reviewed | Last reviewed by Ernest Hawk, M.D., on January 27, 2025
Most cases of mesothelioma are caused by exposure to a substance called asbestos. This rare cancer develops in the mesothelial cells, the thin layer of tissue that lines the chest cavity and is also known as the pleura.
But what is asbestos? How might you be exposed to it? And, is there anything you should do to lower your risk of developing asbestos-related cancers?
We spoke with Ernest Hawk, M.D., vice president and head of Cancer Prevention and Population Sciences. He’s what he shared.
What is asbestos, and how might the average person be exposed to it?
Asbestos is a group of six naturally occurring mineral fibers that have special properties, such as being fire resistant and good insulators. They are found in certain types of rock and extracted through mining. Their names are:
- Actinolite
- Amosite
- Anthophyllite
- Chrysotile
- Crocidolite
- Tremolite
Until the 1970s, asbestos was used a lot in manufacturing. It could be found in everything from roof shingles and brake pads to flooring and insulation. Once asbestos was identified as a carcinogen, though, government agencies stepped in to start limiting its use. They also developed strict protocols on how materials containing asbestos could be handled, removed and disposed of.
Asbestos exposure is not considered as much of an issue today because its use has declined so much in the past 50 years.
Is there anything I should do to reduce my risk of asbestos exposure?
For the most part, no. Asbestos finds its way inside our bodies primarily through respiration. In other words, we breathe in the fibers and dust when we’re exposed to ore or other materials containing asbestos, and they get caught inside our lungs.
Small amounts of asbestos are still used in some products and industries today. But the average person probably won’t encounter it in high enough concentrations to increase their risk of developing a related cancer.
Prolonged, repeated exposure to asbestos is required for cancer to become an issue. That’s why people who lived or worked close to Ground Zero after the 9/11 World Trade Center attacks are at increased risk. And, anyone involved in the renovation or demolition of older residential or commercial structures could also be exposed to asbestos.
But unless you’re a miner, auto mechanic, roofer or construction laborer who worked in those industries mostly before about 1970, your risk is pretty low.
Which cancers are caused by asbestos exposure?
Mesothelioma is by far the most common. But asbestos exposure has also been linked to lung cancer, laryngeal cancer, ovarian cancer and even some gastrointestinal cancers.
Interestingly, asbestos was a factor in the recent lawsuits linking talcum powder to ovarian cancer, too. I’ve often wondered how something that's primarily inhaled can get so far inside the body. Maybe that connection will someday become clearer.
Are there any warning signs or symptoms of asbestos exposure?
No. That’s one of the challenges. There weren’t any screening tests to look for asbestos-related cancers in otherwise healthy individuals back in the 1970s. There still aren’t today. That’s why these cancers tend to be found in more advanced stages.
How are asbestos-related cancers usually diagnosed?
Mesothelioma and lung cancers caused by asbestos exposure are normally diagnosed with a chest X-ray in someone who complains of shortness of breath, trouble breathing, persistent coughing or other symptoms.
Why does asbestos exposure cause cancer?
There are currently three theories:
- Chronic inflammation
- Changes in cell signaling, or how our cells communicate with one another
- Free radicals, or highly unstable oxygen molecules that can damage cell DNA
But none of these offers a really satisfying explanation. So, it’s still a bit of a mystery.
Are there any unique features to help identify asbestos-related cancers?
No. I’ve seen reports that researchers are exploring potential blood markers. But it’s all still very experimental, so there’s nothing definitive yet. And, there are no distinctive, signature mutations related to asbestos exposure that I know of.
Even when we find actual asbestos particles in a biopsy specimen and can infer that it played a major part in causing a cancer, it doesn’t really influence treatment, as there is no treatment tailored to it.
What’s the most important thing to know about asbestos and cancer?
This is one instance in which government regulation has been really helpful. There’s always a bit of second-guessing involved at the beginning of that process, when you wonder, “Are we overdoing this?”
But there’s no doubt now that asbestos regulation has significantly decreased the incidence of all exposure-related diseases, including cancer. Recognizing the link between asbestos and cancer — and then acting on it by removing the source of exposure — has proven to be a highly effective prevention strategy.
Request an appointment at MD Anderson online or call 1-877-632-6789.

The average person won’t encounter enough asbestos to increase their risk.
Ernest Hawk, M.D.
Physician