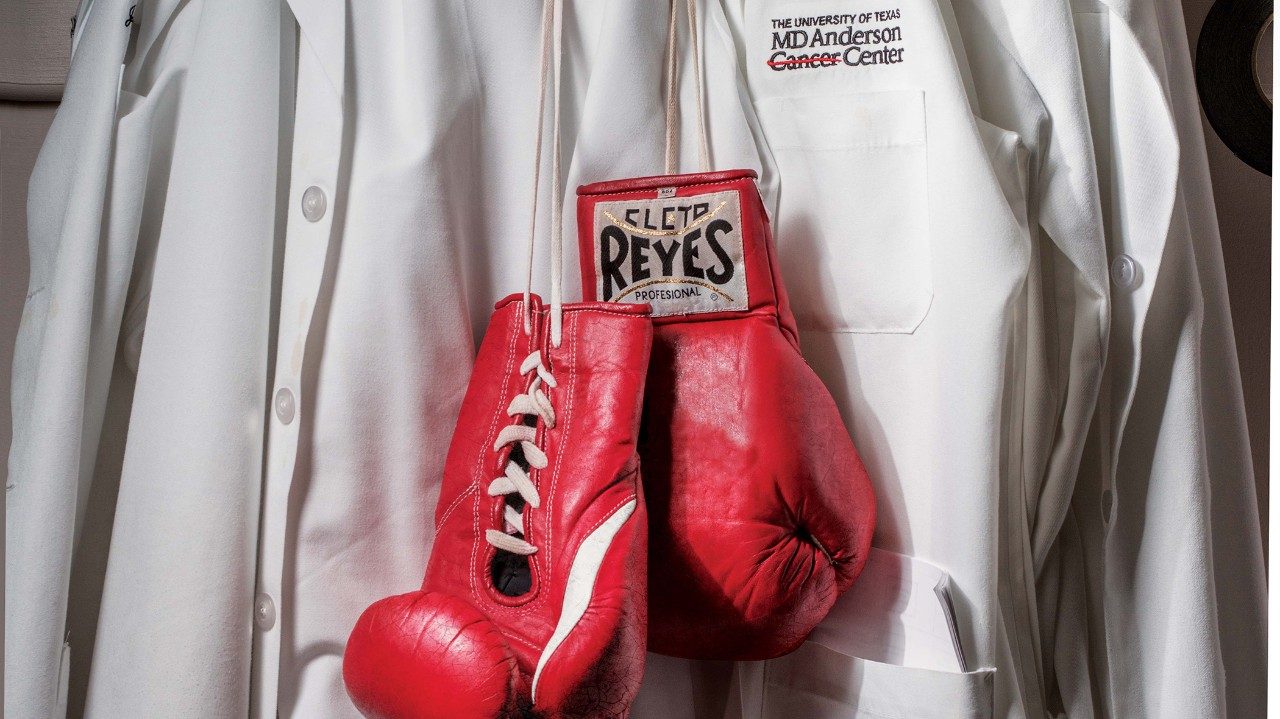
“What’s next in the fight against tobacco?”
That’s the question we asked some of MD Anderson’s experts on tobacco control. Here’s what they told us ...

Alexander Prokhorov, M.D., Ph.D.
Professor in Behavioral Science
Fifty years ago, cigarettes dominated the market. Now we’re also dealing with a wide variety of new products — e-cigarettes, snus (moist tobacco placed under the upper lip that doesn’t require spitting) and hookahs (water pipes) — that often are marketed as ‘safe.’ Impactful and sustainable educational programs need to be designed, tested and broadly implemented so that the public, especially young people, understand the consequences of using both conventional and new products.

Ellen R. Gritz, Ph.D.
Chair of Behavioral Science
What’s needed most is a comprehensive and concentrated approach to tobacco use. Among other things this approach would include attention to disparities in underserved groups such as the poor, less educated, and those with mental health and substance abuse diagnoses. We need greater state funding of tobacco prevention and cessation programs (from monies provided by the settlements with the tobacco industry). And the “will” of city, state and federal legislators to impose significantly higher taxes on any form of tobacco use.

Mark Moreno
Vice president for governmental relations
Over the past 50 years, health care and community advocates and policy makers have made significant progress toward reducing the tremendous burden of tobacco-related diseases through legislative and regulatory policy changes (i.e., high excise taxes on tobacco products, stringent marketing restrictions). While comprehensive approaches such as statewide smoke-free legislation are sometimes resisted, the advocacy community has persisted with success by adopting local ordinances. Eliminating tobacco-related illnesses will require even more creative and tireless efforts such as these.

Lewis Foxhall, M.D.
Vice president for health policy
Over the past 50 years, smoking rates have been cut in half, but we need to take what we’ve learned and act now to protect the next generation from the illness and suffering that are completely preventable.

Maher Karam-Hage, M.D.
Associate professor in Behavioral Science
I hope we can see an end to smoking very soon. It shortens life by about 10 years. However, quitting by age 40 can reduce that by 90%. Even quitting by age 60 can reduce those 10 years by half. Today we have excellent treatments for those who want to quit. We have new and safer ways of delivering nicotine to those who are addicted and can’t quit smoking.

Ernest Hawk, M.D.
Vice president and head of Cancer Prevention and Population Sciences
“Progress” is no longer our primary goal. We’re striving for a cultural transformation that promotes the health and wellness of our entire community. In that vision, tobacco has no place. This will be achieved through the prioritization of the public’s health; commitment to collaborations; implementation of comprehensive, evidence-based actions; and compassionate assistance for tobacco users who want to stop.

Paul Cinciripini, Ph.D.
Professor in Behavioral Science
Improve tobacco control by bolstering the FDA’s newly acquired regulatory authority over tobacco products with empirical research and, most importantly, convince government leaders to extend this authority to all products that contain nicotine, including e-cigarettes. We need to extend our treatments to the most vulnerable in our population, including the disadvantaged and underserved and particularly people with mental health and substance abuse problems.

Ron DePinho, M.D.
MD Anderson president
Of the 94 million former and current smokers, 88% started smoking as children. But I’m energized by the traction we’ve gained on numerous fronts. Thanks to our philanthropy-supported Moon Shots Program, we have organized an aggressive, wide-ranging tobacco control effort encompassing a unique institutional initiative, EndTobacco, which spans childhood prevention programs, adult cessation services and public education and policy collaborations. We’ll build on the momentum gained in recent years to further reduce access to and interest in tobacco products while further empowering current tobacco users to quit for good.

David Wetter, Ph.D.
Chair of Health Disparities Research
Given that smoking has become increasingly concentrated in populations with low socioeconomic status, new interventions and policy initiatives must concentrate on reaching these underserved populations.

Jennifer Irvin Vidrine, Ph.D.
Associate professor in Health Disparities Research
People with limited economic resources are vulnerable and more likely to smoke and tend to have greater difficulty quitting. We need to focus our efforts on treating them.