MD Anderson is helping an at-risk group beat nicotine addiction
People with psychiatric disorders are more likely to be smokers. A new program is training community health providers to deliver tobacco cessation services.

Photo: Wyatt McSpadden
More than 50 years after the U.S. Surgeon General first warned about the dangers of cigarettes, smoking rates have plummeted.
Yet despite irrefutable evidence that smoking causes cancer and other diseases, 15% of the population still smokes. A number of these smokers are people with what is commonly referred to as a mental health condition, such as schizophrenia or bipolar disorder. Many experts now refer to these conditions as behavioral health disorders — a term that collectively describes mental illness and substance use disorder. People who suffer from these types of conditions make up almost 50% of the U.S. tobacco market.
“The smoking rate for people with behavioral health disorders is about two times higher than for those without such conditions,” says Janice Blalock, Ph.D., associate professor of Behavioral Science.
According to the Centers for Disease Control and Prevention, one in five U.S. adults has some form of behavioral health disorder, and 35 to 69% smoke cigarettes. In comparison, 15% of adults without such conditions are cigarette smokers.
“Smokers with behavioral health needs die 25 years younger than the general population, primarily of tobacco-related illnesses,” Blalock says. “They smoke more heavily and more intensely, meaning they’re getting a lot more of the negative stuff from tobacco.”
Helping those diagnosed with such disorders quit smoking hasn’t been a priority, until now.
“Because some health care providers and facilities are more focused on treating their patients’ psychiatric diseases,” Blalock says, “they may not consider treating tobacco addiction.”
Some providers have feared that taking tobacco away might worsen patients’ conditions, and some facilities have even offered cigarettes as rewards for good behavior, she says.
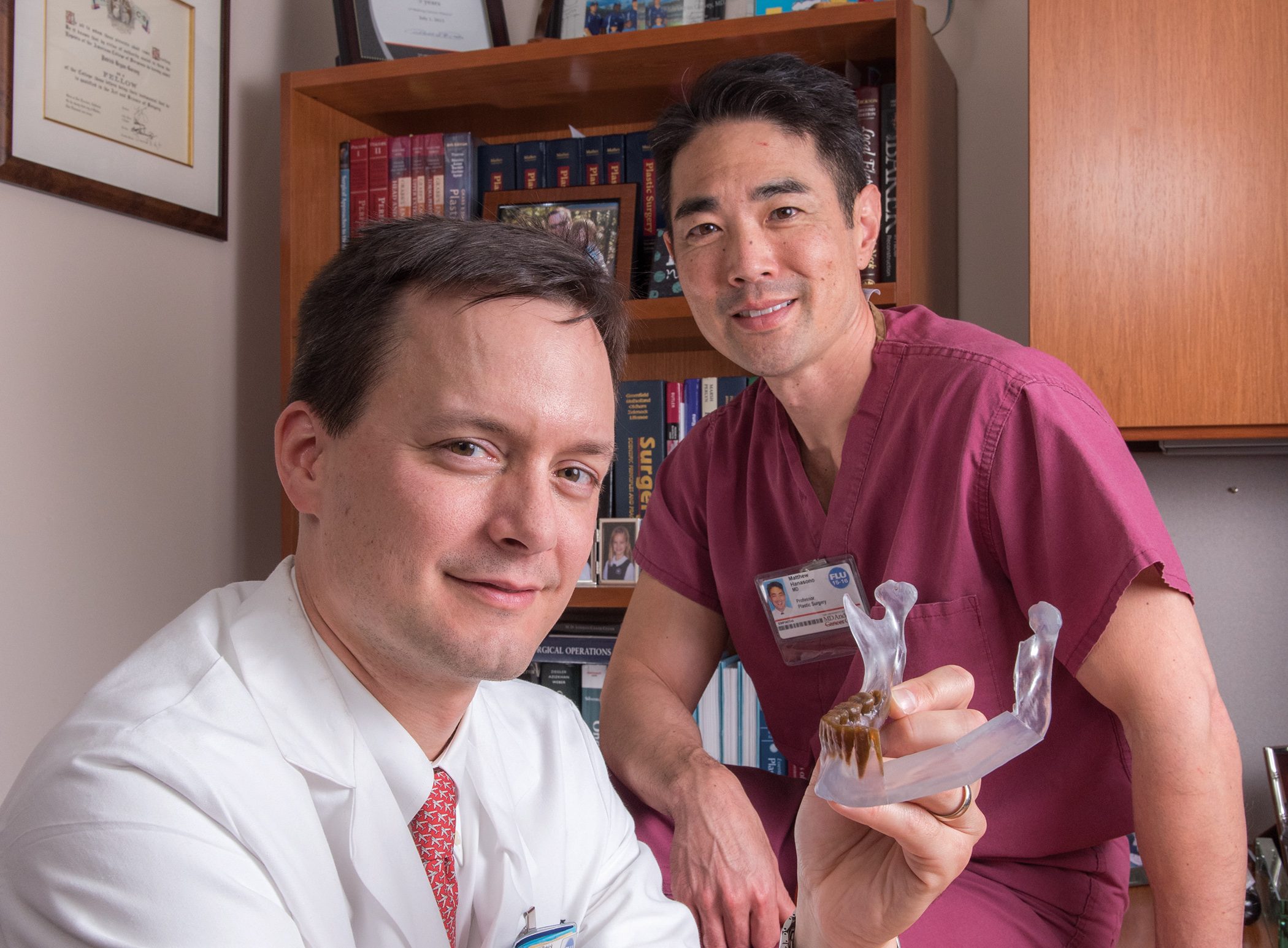
Blalock and Cho Lam, a senior faculty fellow in Psychology at Rice University, co-lead a program called Project TEACH (Tobacco Education and Cessation in the Health System), which trains community providers to deliver tobacco cessation services to behavioral health patients. Launched in 2015, Project TEACH is conducted in partnership with Rice University, the University of Houston and Austin Travis County Integral Care — Travis County’s provider of behavioral health services.
“I’ve been working in the mental health field 31 years and we operated under the misconception that because a person had a mental illness, they couldn’t stop smoking,” says Deborah Shedrick, program manager at Spindletop Center, a community behavioral health clinic based in Beaumont, Texas. “We found out they really did want to stop smoking, but nobody had ever asked them.”
The Spindletop Center is one of seven community behavioral health centers across the state participating in Project TEACH. They’re working with Texas’ Local Mental Health Authorities, organizations that are under contract with the Texas Department of State Health Services to deliver treatment in specific geographic areas of the state.
To connect MD Anderson’s experts with clinics statewide, Project TEACH uses a videoconferencing program called ECHO, or Extension for Community Healthcare Outcomes.
“The ECHO platform is readily available and used at the convenience of clinicians. This allows us to disseminate information effectively without having to visit and train in person,” says Jennifer Cofer, director of EndTobacco, an initiative of the cancer prevention and control platform of MD Anderson’s Moon Shots Program. The platform, along with the Lung Cancer Moon Shot, provides support for Project TEACH.
Using ECHO, counselors and physicians from MD Anderson’s Tobacco Treatment Program meet one hour each week with community providers. Sessions teach them how to help people with behavioral health needs stop smoking, and offer a forum for providers to discuss their most difficult and challenging cases.
Everyone involved learns something, including MD Anderson experts.
“The experts listen to our feedback, and we share,” says Shedrick. “We’re all on the same team.”
Shedrick describes a complete cultural shift at Spindletop Center. She’s seen a number of clients successfully quit or reduce their tobacco use. Their lives, from health to finances, are transformed.
Project TEACH will soon expand to more clinics and provide more in-depth assistance.
“People with these conditions want to quit smoking and can quit, when given the proper assistance,” Blalock says. “The process may take longer and require more intensive interventions, but it can be done.”