Taking on rare soft tissue, bone tumors in the pelvis

Related story: Patients of all ages
In her head, Cathy Helminiak knew that her MD Anderson team could bring her through a complex surgery and long recovery from a chondrosarcoma in her right hip joint.
But it was Helminiak’s heart, filled with the prospect of grandchildren, that finally moved her to commit to it.
Looking back more than four years after she had her right leg amputated at the top of the hip, Helminiak’s head and heart served her well. She is cancer-free and mobile with or without her prosthetic leg, and it’s a good thing because her two toddler granddaughters are on the move, too.
Helminiak had a form of surgery called hemipelvectomy, in which the pelvis and/or sacrum (the lower back part of the pelvis) are removed or reconstructed depending on the size, type and location of the bone or soft tissue tumor. The pelvis not only provides the scaffold for bone, muscle and weight distribution, but it encases the pelvic organs, including the prostate or uterus, the bladder, rectum and the large vessels and nerves that serve the lower extremity.
The bone and soft tissue tumors that call for a hemipelvectomy are rare, and for many adult and pediatric patients, finding a skilled surgical team to tackle their cases and save their legs can be a challenge.
The eight- to 16-hour surgeries are difficult unto themselves, but a patient’s post-surgery recovery and rehabilitation also are demanding.
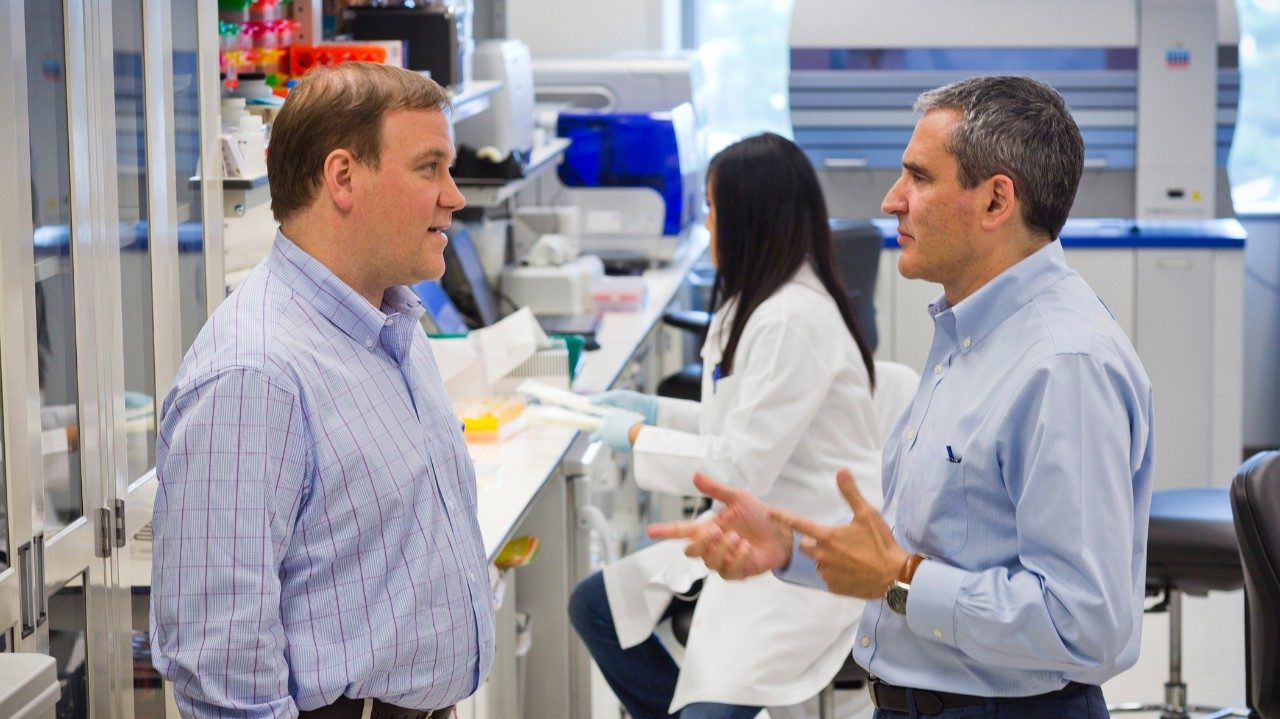
Teamwork essential to rare surgery
Two years ago, Valerae Lewis, M.D., associate professor in the Department of Surgical Oncology and chief of Orthopaedic Oncology, launched the Multidisciplinary Pelvic Sarcoma Surgery Program.
This entity formally brought together a group of specialized surgeons, anesthesiologists, nurses, technicians and rehabilitation specialists, creating a single go-to team for patients who face hemipelvectomies. Together, the team performs all of MD Anderson’s 30 to 50 cases per year.
Lewis says the formalized program has brought a new dimension of collegiality, communication and calm to the operating room. For the patient, the cohesion has reduced time under anesthesia and in the Intensive Care Unit after surgery. A prospective study is underway to determine how the dedicated team ultimately influences outcomes.
“Hemipelvectomies are complicated surgeries for our patients, but they also are physically and mentally tough for the entire surgical team,” Lewis says. “With a designated team that works together frequently, a patient can have great confidence in a team that has great confidence in each other.”