Advancing quality surgical care

It would be easy for surgeons at the top-ranked institution in cancer care to rest on their laurels. But within MD Anderson’s Division of Surgery, a team of physicians and clinical nurse reviewers has determined that room for improvement always exists.
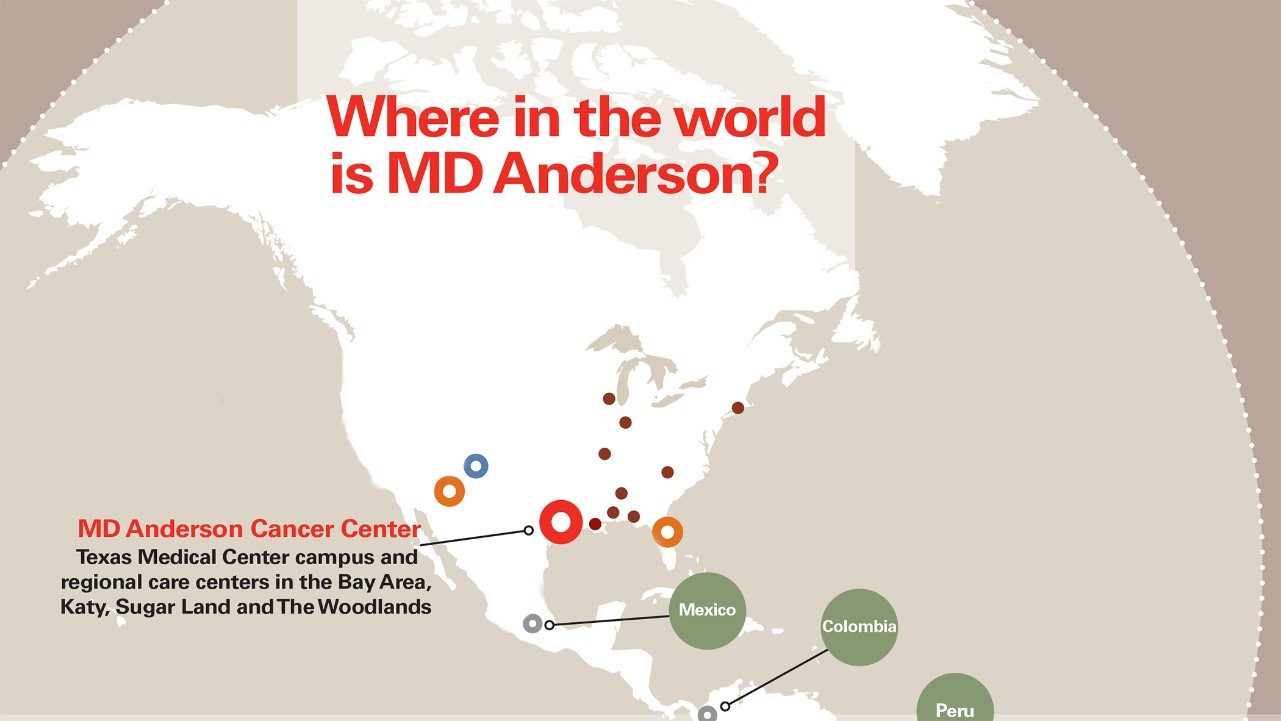
In 2011, MD Anderson began participating in the National Surgical Quality Improvement Program (NSQIP), sponsored by the American College of Surgeons. More than 500 hospitals, including the 41 National Cancer Institute-designated comprehensive cancer centers, are on board.
The program tracks surgical patients for 30 days — even beyond discharge — and records instances of mortality, morbidity (cardiac complications, pulmonary problems, wound issues, etc.), reoperation and readmission. That data is then compared against national standards.
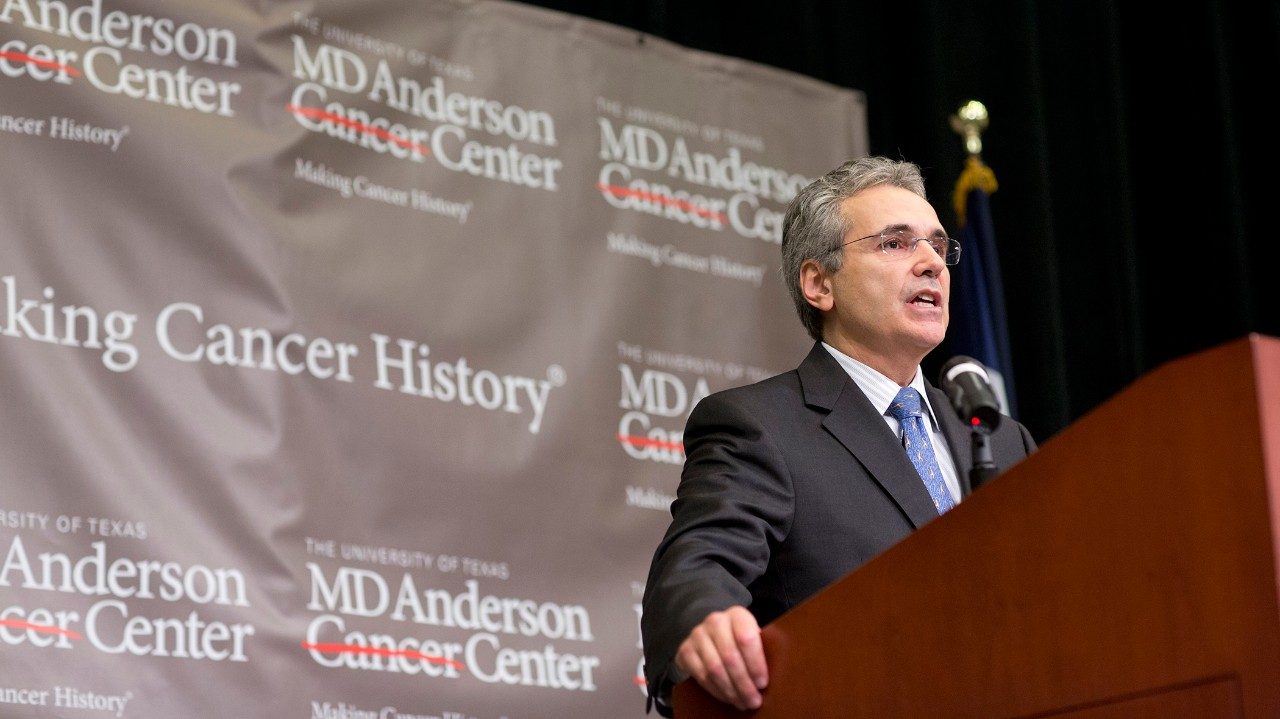
“Participating in this program is a great way to measure our outcomes against the country’s other surgical institutions,” says Thomas Aloia, M.D., assistant professor in the Department of Surgical Oncology. “Comparably, our data reflects many strengths, but there are always opportunities to be better.”
Aloia and his team are now working with other cancer centers to track the influence of risk factors unique to cancer patients: previous chemotherapy, radiation, operations and/or the involvement of multiple surgical specialties.
“NSQIP has done much to advance the quality of surgical care,” Aloia says. “Our hope is to take that model and refine it for surgical oncology."
Doctors and nurses become voice of patient
In early 2012, the Division of Surgery and the Perioperative Enterprise team developed a surgical safety checklist to reduce mortality and surgery-related complications.
Studies show that standardization and formalization of accepted surgical safety practices can save lives and prevent unnecessary complications. Early pilot efforts at MD Anderson proved successful, and the checklist was rolled out to the institution in summer 2012.
“It’s more than fostering a general culture of safety, though that’s certainly a big part of it,” says Charles Levenback, M.D., professor and deputy chair of MD Anderson’s Department of Gynecologic Oncology and Reproductive Medicine. “It’s about recognizing patient-specific risks and taking every precaution against them.”
The checklist is divided into four sections:
- patient entry to the operating room (OR),
- prior to incision,
- prior to closure, and
- prior to surgeon leaving the OR.
The team confirms verifiable items — patient identity, known allergies, procedure site — and discusses important topics related to a successful surgery, such as the anesthesia plan, availability of blood products and potential difficulties.
“The checklist is just a starting point,” Levenback says. “Everyone in the OR needs to feel comfortable speaking up about safety issues. It’s those moments when our patients don’t have a voice that we must be the voice for them.”
DID YOU KNOW?
For its efforts in controlling health care-associated infections in the Intensive Care Unit, MD Anderson received the Outstanding Achievement and Leadership Award from the U.S. Department of Health and Human Services and Critical Care Societies Collaborative in May 2012.