MD Anderson Research Highlights for February 23, 2022
Featuring PIK3CA and FGFR targeted therapy advances, new treatments for myelofibrosis, and laboratory discoveries in pancreatic cancer, glioblastoma and CLL
MD Anderson News Release February 23, 2022
The University of Texas MD Anderson Cancer Center’s Research Highlights provides a glimpse into recently published studies in basic, translational and clinical cancer research from MD Anderson experts. Current findings include targeted therapies for tumors with PIK3CA and FGFR mutations, a promising combination therapy for myelofibrosis, a new target to improve immunotherapy response in pancreatic cancer, a novel method of increasing chemoradiation sensitivity in glioblastoma, and greater understanding of the chronic lymphocytic leukemia immune microenvironment.
Copanlisib shows activity against tumors with PIK3CA mutations
PIK3CA is the most commonly mutated oncogene, with mutations found in several cancer types, including liver, breast, colon, ovarian, gastric, brain and lung. As part of the NCI MATCH trial, Senthil Damodaran, M.D., Ph.D., led the evaluation of copanlisib — a class 1 pan-PI3K inhibitor with activity against both the alpha and delta isoforms of the protein — in patients with PIK3CA mutations with or without PTEN loss. In the analysis of 25 patients, the overall response rate was 16%, meeting the primary endpoint of the study. Most of the patients had multiple prior treatments, with 68% having received three or more lines of prior therapy. In contrast to other PI3K inhibitors, copanlisib was well tolerated. The results suggest that copanlisib could be a feasible therapeutic option for select tumors with PIK3CA mutations, either alone or in combination approaches. Read more in the Journal of Clinical Oncology.
Examining the safety and efficacy of navitoclax and ruxolitinib for myelofibrosis
Myelofibrosis is a cancer of the bone marrow that causes severe anemia and can progress to acute leukemia. The most commonly available targeted therapy for higher risk myelofibrosis is ruxolitinib, a JAK inhibitor, but cancers can develop resistance to JAK inhibitors over time. Preclinical models demonstrated that targeting the BCL-XL pathway can overcome JAK inhibitor resistance. A Phase II trial led by Naveen Pemmaraju, M.D., investigated the safety and efficacy of combining ruxolitinib with navitoclax, a BCL-XL/BCL-2 inhibitor, for patients with progressive or resistant disease. Of 34 patients receiving the combination therapy, 41% experienced spleen volume reduction, while 30% experienced a 50% or more reduction in total symptom score. Of 11 evaluable trial participants with anemia, 64% saw improvement. At a median follow-up of 21.6 months, the median overall survival was not yet reached. The most common side effect was reversible thrombocytopenia, occurring in 88% of trial participants. Future research will examine the combination’s potential to improve patient outcomes. Learn more in the Journal of Clinical Oncology.
FGFR inhibitor pemigatinib demonstrates safety and clinical activity in patients across tumor types with FGFR alterations
Dysregulated fibroblast growth factor receptor (FGFR) signaling, as a result of FGFR alterations, has been implicated as an oncogenic driver in numerous malignancies. In the international Phase I/II FIGHT-101 study, Vivek Subbiah, M.D., and a team of researchers examined the safety and preliminary efficacy of pemigatinib, a potent and selective FGFR inhibitor, for refractory advanced malignancies with and without fibroblast growth factor (FGF) and FGFR alterations. The drug achieved responses across tumors, with a partial response rate of 9% — most commonly in cholangiocarcinoma, as well as head and neck, pancreatic, gallbladder and uterine tumors. Overall response rates were 25% and 23.1% for patients with FGFR fusions or rearrangements and FGFR mutations, respectively. The findings showed that pemigatinib was associated with a manageable safety profile and clinical activity, prompting a registrational study in cholangiocarcinoma and further Phase II/III trials, demonstrating the benefit of precision therapy even in early phase trials. Learn more in Annals of Oncology.
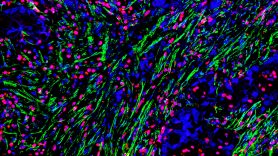
Targeting HIF2 may be novel strategy to improve immunotherapy response in pancreatic cancer
Pancreatic cancer resides within a dense network of scar-like tissue called stroma that shields the cancer from chemotherapy and immunotherapy. Tumor stroma is very low in oxygen, and this stress stabilizes proteins called hypoxia-inducible factors (HIF1 and HIF2), which are thought to contribute to therapeutic resistance and aggressive growth. In a new preclinical study, researchers led by Carolina Garcia Garcia, Yanqing Huang, Ph.D., Natividad Fuentes, Ph.D., and Cullen Taniguchi, M.D., Ph.D., discovered that loss of stromal HIF2, but not HIF1, delayed pancreatic cancer progression and enhanced survival of laboratory models. The research team found that HIF2 acts within stromal cells called cancer-associated fibroblasts to recruit M2-polarized macrophages and regulatory T cells, which both suppress anti-tumor immunity. Blocking the activity of HIF2 with a class of FDA-approved inhibitors enhanced the activity of immune checkpoint inhibitors in preclinical studies. These findings suggest that HIF2 is a potential therapeutic target to enhance responses to immunotherapy in pancreatic cancer. Learn more in Gastroenterology.
New study targets DNA repair and survival pathways to restore chemoradiation sensitivity to treat GBM
The current standard-of-care treatment for patients with glioblastoma (GBM) is surgical resection followed by radiation therapy with concurrent and adjuvant temozolomide. However, despite aggressive treatment, the median survival for patients with GBM remains less than two years. Homologous recombination (HR), a DNA repair pathway, can facilitate resistance to chemoradiation in glioma stem cells. Therefore, Vinay Puduvalli, M.D., and a team of researchers evaluated the safety and efficacy of targeting heat shock protein 90 (HSP90) — a molecular chaperone that plays a critical role in the function of key HR proteins — to compromise HR. Using laboratory models of GBM, researchers demonstrated that onalespib, a brain-penetrating HSP90 inhibitor, promoted degradation of its client proteins and augmented the efficacy of chemoradiation in vitro and in vivo. HSP90 inhibition also reprogrammed the transcriptome and proteome, modifying known and novel client proteins, which may serve as additional therapeutic targets for combination therapies. These findings provide a strong rationale for assessment of HSP90 inhibitors in combination with chemoradiation therapy in patients with GBM. Learn more in Clinical Cancer Research.
T-follicular helper cells play key role in CLL cellular proliferation
In chronic lymphocytic leukemia (CLL), B lymphocytes proliferate in the blood, bone marrow and lymph nodes. Specific classes of T cells are essential for B-cell expansion, and malignant CLL cells are thought to require help from these T cells to proliferate within lymph nodes. Researchers led by Jan Burger, M.D., Ph.D., studied the cellular and molecular interactions between CLL and T-helper cells using nurse-like cell (NLC) co-cultures as a model of the CLL lymph node microenvironment. By examining cultures from 28 patients with CLL, they demonstrated that both T-follicular helper cells (Tfh) and regulatory T cells (Treg) expanded in the NLC cultures. Additional analysis showed that Tfh, but not Treg, tend to be found alongside proliferating CLL cells, suggesting cross-talk between these cells. Future validation of this model may allow development of new therapies for CLL that target key Tfh molecules, like CD40L, IL-21 or CXCR5. Learn more in Leukemia.
In case you missed it
Read below to catch up on recent MD Anderson press releases.