- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (230)
- Breast Cancer (720)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (114)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (8)
- Kidney Cancer (128)
- Leukemia (344)
- Liver Cancer (50)
- Lung Cancer (288)
- Lymphoma (284)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (174)
- Pancreatic Cancer (164)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (96)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (632)
- Complementary Integrative Medicine (24)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (914)
- Research (398)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (608)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (322)
- Symptoms (184)
- Treatment (1790)
What’s new in leukemia research?
5 minute read | Published May 29, 2024
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on May 29, 2024
Leukemia is an overarching term encompassing several subtypes of blood cancers. Blood cells are produced in the bone marrow, the spongy material inside bones. The bone marrow contains immature stem cells that develop and mature to become red blood cells, platelets, or different types of white blood cells.
When mutations occur in bone marrow stem cells, it can interfere with the body’s normal production of blood cells. This can start as a disease or disorder classified as a pre-leukemia state (and may or may not progress to leukemia), or it can start as leukemia.
Fadi Haddad, M.D., assistant professor of Leukemia, walked us through a few updates in leukemia research being presented at the 2024 American Society of Clinical Oncology Annual Meeting (ASCO).
Oral use of a known drug to treat myelodysplastic syndrome
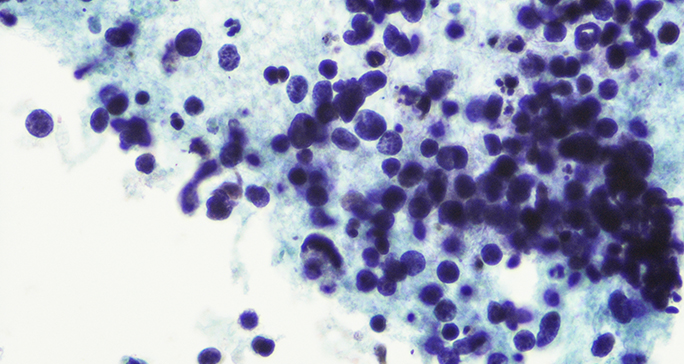
Myelodysplastic syndrome (MDS) is a pre-leukemia state. Haddad explains, “Myelo means related to the bone marrow, and dysplasia means abnormal growth. So, in patients with MDS, the bone marrow is abnormal. If left untreated, it could progress to acute myeloid leukemia (AML).”
Azacitidine is approved as a treatment for MDS. “It’s given either as an intravenous (IV) infusion, or it's given as subcutaneous injections, meaning under the skin,” says Haddad. Both options could be inconvenient for some patients. “The IV infusion requires patients to come to the hospital repeatedly as long as they are receiving the treatment. The subcutaneous injections can be done at home, but they can cause hematomas and pain in the skin at the site of the injection.” Compounding the inconvenience, patients may receive the treatment for several months or years.
In a study (Abstract 6509) presented by Guillermo Garcia-Manero, M.D., professor of Leukemia, researchers looked at the safety and efficacy of taking azacitidine orally, rather than via infusion or injection, for patients with low- or intermediate-risk MDS. While azacitidine taken orally is approved for maintenance therapy in patients with AML in remission, it is not currently approved for the treatment of MDS.
The study found that oral delivery of azacitidine had side effects similar to what we’ve seen with oral azacitidine in previous studies. The preliminary efficacy of the drug was also good. “Close to 30% of patients saw hematologic improvement, which supports the continued evaluation of oral azacitidine in low- or intermediate-risk myelodysplastic syndrome,” Haddad notes.
An investigational drug for acute myeloid leukemia (AML) treatment
One area of interest in AML research is refining treatment both for older patients who need lower intensity treatment and for patients with AML that has come back (relapsed) or is not responding to treatment (refractory). The current standard of care is a combination of the drug venetoclax with either azacitidine or decitabine.
“We've been investigating several compounds that are added to one of these combinations,” Haddad notes. A study (Abstract 6511) presented by Maro Ohanian, D.O., associate professor of Leukemia, looks at the preliminary results of a clinical trial combining standard venetoclax and decitabine treatment with a new drug called BP1001. “Adding BP1001 is supposed to enhance the cancer cell sensitivity to chemotherapy, so the effect of the chemotherapy will be stronger,” says Haddad.
The study looked at this three-drug combination in older patients with newly diagnosed AML as well as in patients of all ages with relapsed or refractory AML. “This triplet combination was safely administered to patients in both groups without new or unexpected toxicities,” Haddad summarizes. “The study is continuing enrollment and will expand to enroll more patients to collect data on efficacy.”
Examining safety concerns for bone marrow transplants following treatment of AML with a known compound
Another treatment option for some subtypes of AML is a drug called gemtuzumab ozogamicin (GO). GO is a type of molecule known as an antibody drug conjugate. This means that two parts make up GO: an antibody that attaches to a biomarker on cancer cells and a chemotherapy drug. “When we give patients this kind of treatment, the antibody attaches to the leukemia cell, and the drug enters the leukemia cell and leads to its death,” Haddad explains.
The Food and Drug Administration (FDA) approved GO in 2017, but there have been concerns about side effects for patients who take GO and later receive bone marrow transplants. “One of the side effects that we should pay attention to is hepatotoxicity — negative impacts to the liver. In rare cases, it can cause hepatic veno-occlusive disease, or VOD. This is a very serious condition that can lead to liver failure if left untreated,” says Haddad. Patients who take GO may be at a higher risk of developing VOD when they go on to receive bone marrow transplants.
To investigate these safety concerns, Partow Kebriaei, M.D., professor of Stem Cell Transplantation, led a multi-center effort to collect and analyze data (Abstract 6516) from adult patients with AML who received GO and went on to undergo bone marrow transplantation. “The rates of VOD and the rates of mortality are similar to patients who got a transplant but did not take GO,” says Haddad. “This means the drug did not add much toxicity compared to what we see without the drug, and GO appears to be safe for use.”
Factors in myelofibrosis outcomes, treatments for chronic lymphocytic leukemia, and more
Two other research talks come from William Wierda, M.D., Ph.D., professor of Leukemia, and Julie Braish, M.D., a fellow in Leukemia. Wierda led the CAPTIVATE Phase II clinical trial (Abstract 7009). This trial looked at the combination of venetoclax and ibrutinib in patients with chronic lymphocytic leukemia and small lymphocytic lymphoma. Braish, working with Lucia Masarova, M.D., assistant professor of Leukemia, examined factors affecting outcomes in patients with myelofibrosis, another pre-leukemia state (Abstract 6514). These factors include the variant allele frequency of the JAK2 gene mutation and the presence or absence of cytopenias (lower than normal blood cell counts).
In addition to these presentations, MD Anderson researchers are giving two other oral presentations and numerous posters on leukemia research at the 2024 American Society of Clinical Oncology Annual Meeting. “Our presentations at ASCO represent the impact our research is having in pushing a really broad range of leukemia and pre-leukemia research and treatment forward,” says Haddad.
Learn about research careers at MD Anderson.

Researchers at MD Anderson are developing multiple therapies and combination strategies and tackling different disease subgroups of leukemias and myeloid disorders.
Fadi Haddad, M.D.
Physician & Researcher