- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (632)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (918)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (322)
- Symptoms (182)
- Treatment (1786)
Chronic versus acute leukemia: Different diagnoses, different treatments
BY Devon Carter
5 minute read | Published June 09, 2021
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on June 09, 2021
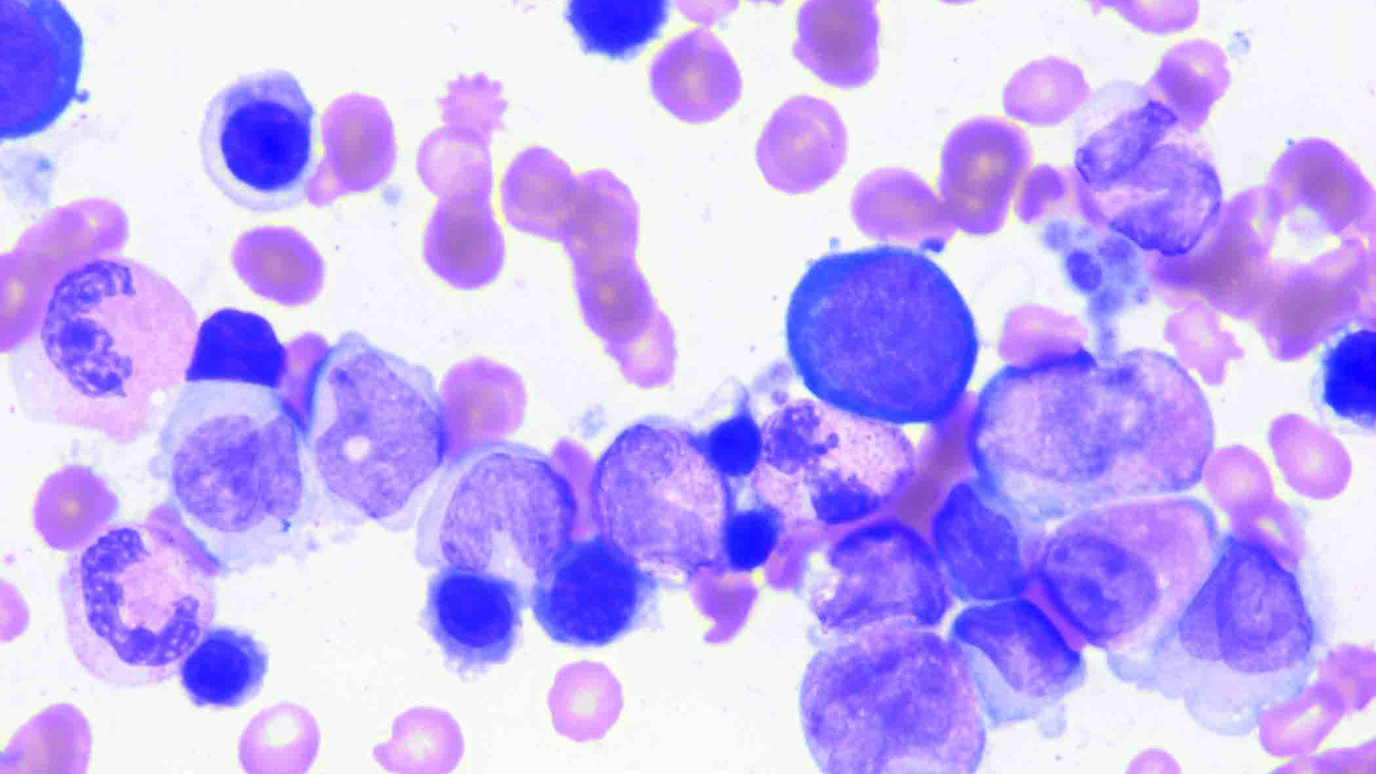
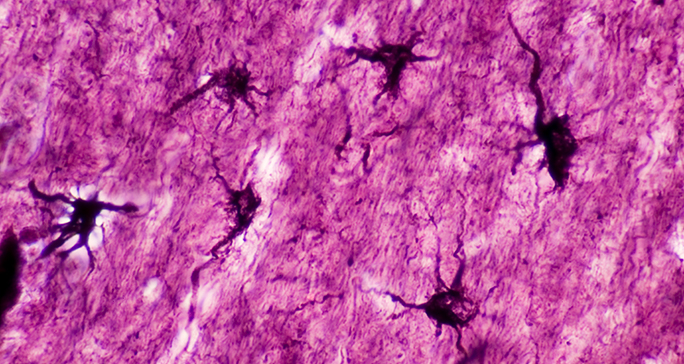
Stem cells come from our bone marrow and grow to become red blood cells, white blood cells and platelets. These cells make up our blood and play vital roles in our health by transporting oxygen to our organs, helping to fight infections and stopping bleeding if we’re cut.
If these cells stall in their development, it can result in leukemia. Depending on the type of stem cells damaged and when the breakdown in their growth occurs, leukemia can be classified into two groups: acute or chronic.
Our Elias Jabbour, M.D., shares the differences in acute and chronic leukemias, including how they’re subtyped and how that helps determine treatment.
What is the difference between acute and chronic leukemia?
Like all living things, cells have a life cycle: They’re born, mature and then die. With leukemia, there’s a blockage in that life cycle. The baby cells don’t mature, or the adult cells never die. Leukemias are classified based on when the cells deviate from in their life cycle.
- Chronic leukemia results from a failure in the life cycle after the cells have matured. The adult cells are often able to still function to some extent, but, ultimately, they’re not compatible with life.
- Acute leukemia occurs when there’s a halt in development early in the cell life cycle. These stumped baby cells have zero function.
How do lymphoid cells or myeloid cells fit into a leukemia diagnosis?
Beyond chronic and acute, a leukemia diagnosis can be further defined by determining which of the two types of stem cells are affected: lymphoid cells or myeloid cells.
Lymphoid cells produce lymphocytes, which are white blood cells that make up a large part of the immune system. Myeloid cells produce red blood cells, platelets and other types of white blood cells that aren’t lymphocytes.
Although there are rarer forms of the disease, most leukemias fall into four main subtypes:
- acute myeloid leukemia
- acute lymphoblastic leukemia
- chronic myeloid leukemia
- chronic lymphocytic leukemia
No matter when the malfunction occurs in the life cycle and which cells are affected, the cancer cells crowd out healthy cells and prevent them from carrying out their important jobs.
Do the symptoms differ between chronic and acute leukemias?
Yes, chronic leukemias develop slowly, so most patients don’t experience as many symptoms.
However, patients with acute leukemias typically bleed easily, like when brushing their teeth. They may have frequent nose bleeds or heavier menstruation. Also, they often have experience fever and fatigue.
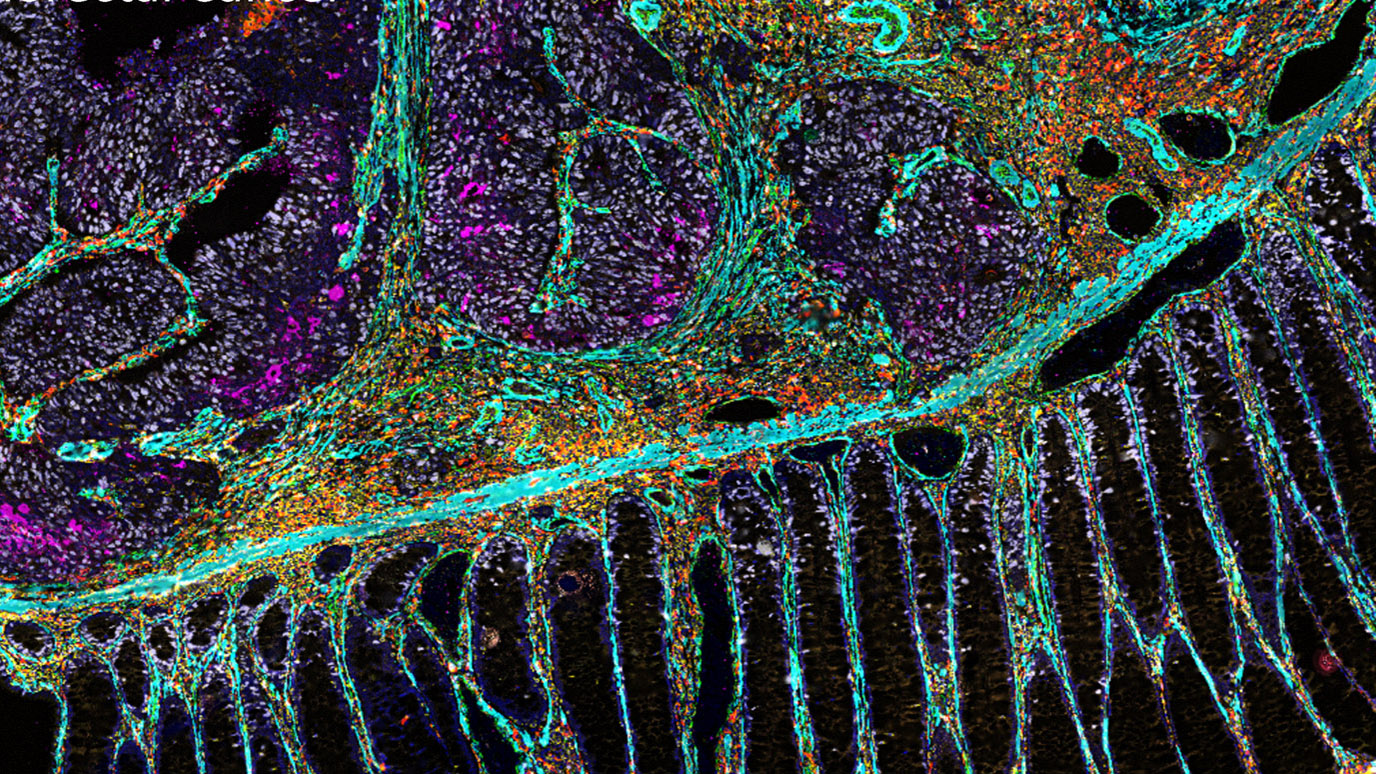
How are acute leukemias treated?
The goal of treatment is to reestablish the normal function of cells. With acute leukemias, the first step is called induction. With chemotherapy, we treat the cancer cells in the blood and also the bone marrow. To ensure all cancerous cells are gone, there is a second step of treatment called consolidation. For this step, some patients receive more chemotherapy and others receive more chemotherapy plus a stem cell transplant. The consolidation approach depends on how aggressive the leukemia is as well as the unique genetic characteristics of the diagnosis, which is determined through a series of tests at initial diagnosis.
The third phase is maintenance, which helps manage the risk of the cancer coming back. For two or three years, patients take chemotherapy mainly as pills and come to the hospital only once a month. We’ve used this approach for some time with treating acute lymphoblastic leukemia, but new research is showing it helps extend the lives of patients with acute myeloid leukemia, too.
Lastly, because some chemotherapies can’t pass through what’s call the blood-brain barrier, we used to use radiation therapy to prevent a relapse there. But it can cause in long-term side effects, which can have a big impact for our pediatric leukemia patients. Now, we use intrathecal chemotherapy, which is injected into the spine and travels up to the brain.
How are chronic leukemias treated?
Any cancer diagnosis is a challenge, but the good news is that with chronic leukemia, you can live a normal life. In fact, 40% of patients with chronic lymphocytic leukemia can just be monitored and don’t need treatment.
When it comes time to treat the cancer, we use targeted therapies since patients with chronic leukemias tend to be older and have more in their medical histories.
Chemotherapy works by killing everything, with the hope that the cancer cells will die and the normal cells will recover. But since it wipes out everything, there’s a period when the patient has a low number of healthy blood cells and faces a risk of complications. Targeted therapies, on the other hand, attack only the cancer cells, sparing everything else and limiting that risk of complications. There are several targeted drugs being used alone or in combination with chemotherapies to treat leukemias now, but there are more on the horizon.
Unfortunately, there isn’t any watching and waiting with chronic myeloid leukemia. But the treatment is a pill. Historically, patients took the pill for the rest of their lives, but newer research shows that if a patient is doing well after five or six years, we can stop the chemotherapy with a low risk of the cancer recurring.
Is there anything else you’d like to share about leukemia treatment?
I'm very excited because I think we’ll cure leukemia in my lifetime. We’ve already come so far. For example, before 2000, patients with Philadelphia chromosome-positive acute lymphoblastic leukemia had a survival rate of 10%. Targeted therapy improved that to 35% to 40%, but patients had to receive a stem cell transplant, which isn’t easy. But I’ve led research on a drug called ponatinib in combination with chemotherapy, and we’ve seen the survival rate jump to 80% without a transplant. Our next goal is to increase the survival rate to 90% and eliminate the need for chemotherapy by using a combination of targeted therapy and immunotherapy.
I’m proud because MD Anderson is leading the way. We developed ponatinib here, and now it’s the international standard. We’re are pioneering chemotherapy-free treatment for these patients.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.

We’ve already come so far.
Elias Jabbour, M.D.
Physician