- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (294)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (96)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (630)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (912)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (320)
- Symptoms (182)
- Treatment (1786)
What causes cervical cancer? 6 questions, answered
3 minute read | Published October 28, 2022
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on October 28, 2022
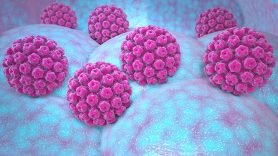
About 10,000 people are diagnosed with cervical cancer each year. The vast majority of cases are due to the human papillomavirus (HPV).
What accounts for the remaining cases of cervical cancer? And can they be prevented? Where do cervical polyps fit into the equation?
To answer these questions and more, we went to Jolyn Sharpe Taylor, M.D., a surgeon specializing in gynecologic cancers. Here’s what she shared.
How many cervical cancer diagnoses are linked to HPV?
The Centers for Disease Control estimates that more than 90% of all cervical cancer cases are caused directly by HPV. That would mean of the 10,000 or so people who are diagnosed each year, more than 9,000 will have cervical cancer because they were exposed to HPV. The remainder would be due to other things.
Which strains of HPV cause cervical cancer?
Approximately half of all cervical cancers are caused by HPV-16. Another 20% are caused by HPV-18. Other strains associated with a higher risk of developing cervical cancer are:
- HPV-31
- HPV-33
- HPV-45
- HPV-52
- HPV-58
If your HPV test comes back positive, it should indicate if the HPV is considered high-risk or not and may specify which strains were found in the sample.
Is there anything else that can cause cervical cancer, besides HPV?
Smoking and being chronically immunocompromised can increase your risk of developing cervical cancer. Also, not having routine cervical cancer screening tests (Pap tests) can mean pre-cancers are not found in time to prevent cancer. Some studies also suggest that oral contraceptives may increase the risk of HPV and eventually cervical cancer, but other factors may be causing that.
Chronic immunosuppression, such as from HIV/AIDS or other disorders of the immune system, is also associated with a higher risk of developing cervical cancer. However, a cancer treatment that only temporarily suppresses the immune system will not increase your risk.
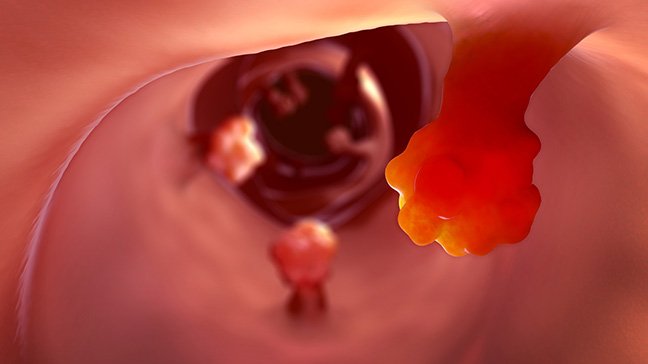
What’s the link between cervical polyps and cervical cancer? Does one lead to the other?
No. There is no connection. Polyps are usually just benign — or harmless — growths of endocervical tissue. They’re not associated with HPV or cervical cancer. But if you have one, you should ask your gynecologist to check it out. Your doctor can decide if a biopsy is necessary to determine whether a cervical polyp is cancerous.
What’s the difference between cervical dysplasia and cervical cancer?
Cervical dysplasia is when cervical cells look abnormal under a microscope. It’s considered a precursor to cancer, or a pre-cancer, and can be caused by HPV.
Cervical dysplasia is very treatable, but there are different grades of dysplasia, based on how abnormal the cells appear under a microscope. When you get a Pap test, your results should be in one of four categories:
- Normal
- Dysplasia/Abnormal and cannot rule out cancer
- Cancer/Carcinoma (either squamous cell or adenocarcinoma)
- Inadequate
Inadequate means that the sample wasn’t big enough to be tested or it was either damaged or unusable. So, results could not be obtained.
Is there anything I can do to prevent myself from getting cervical cancer?
Yes. First, if you’re eligible for an HPV vaccine, get one.
Second, if you’re currently using tobacco products, stop.
And third, get a Pap test or an HPV test with or without a Pap test, as frequently as the current screening guidelines recommend for someone of your age and risk level. That will help your health care provider find cervical cancer early when it’s most treatable.
Those are the three biggest steps you can take to reduce your risk of cervical cancer.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
More than 90% of all cervical cancer cases are caused directly by HPV.
Jolyn Sharpe Taylor, M.D.
Survivor