- Diseases
- Acoustic Neuroma (16)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (18)
- Bile Duct Cancer (26)
- Bladder Cancer (74)
- Brain Metastases (28)
- Brain Tumor (234)
- Breast Cancer (726)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (168)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (130)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (178)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (150)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (300)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (100)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (22)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (238)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (122)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
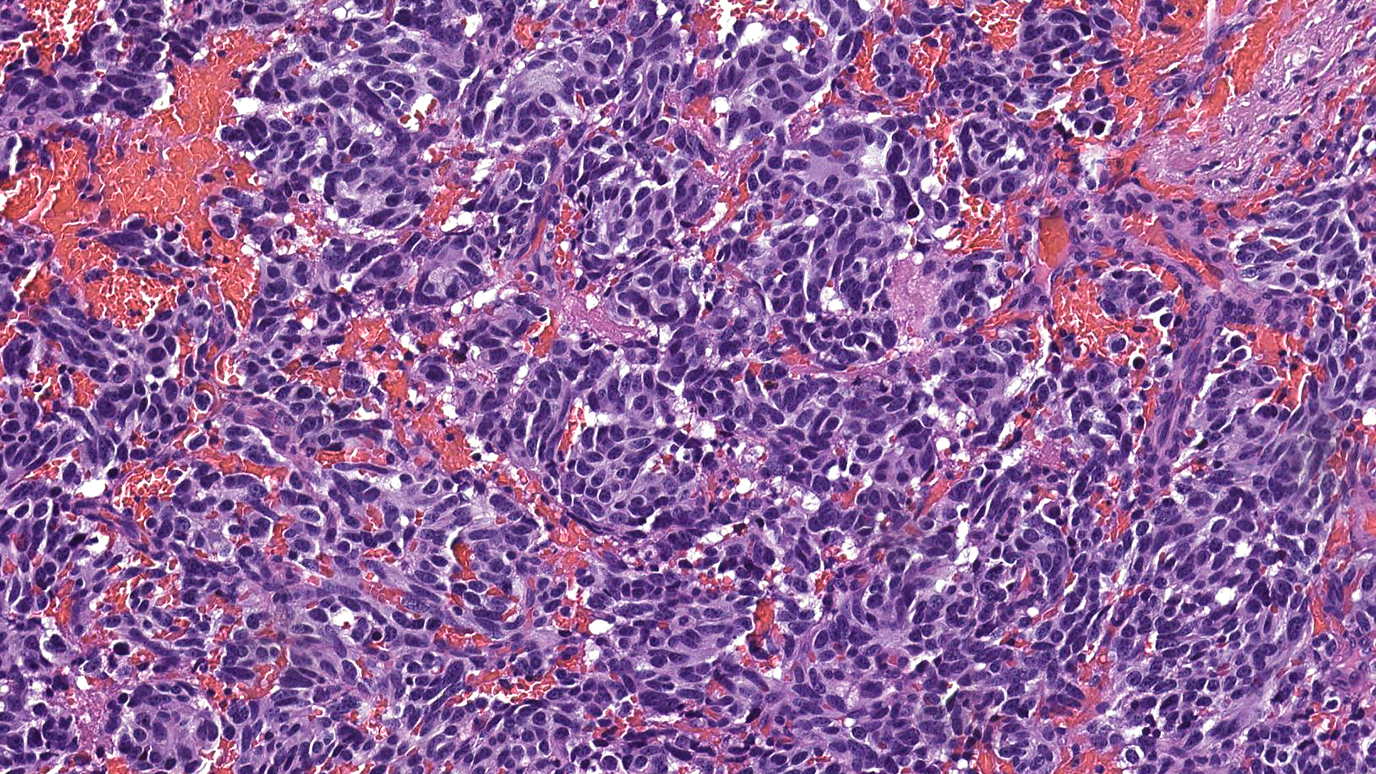
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (936)
- Research (390)
- Second Opinion (78)
- Sexuality (16)
- Side Effects (616)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (408)
- Survivorship (328)
- Symptoms (182)
- Treatment (1788)
5 things women should know about cancer screening
5 minute read | Published September 17, 2019
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on September 17, 2019
When it comes to cancer screenings, some women might think, “Well, I don’t have any symptoms, so I don’t need them.” But that’s actually when you should get them.
Cancer screenings should only be done when you display no symptoms. Otherwise, it’s not a screening test anymore; it’s a diagnostic test. That’s why you shouldn’t wait until you have a lump in your breast or blood in your stool. Because by the time you’re actually showing symptoms, the cancer might not be in its earliest, most treatable stages anymore.
Read on to find out which tests you need and how frequently you should get them, and get answers to other screening questions I often hear at MD Anderson’s Lyda Hill Cancer Prevention Center.
What screenings do I need, and when should I start getting them?
For the average-risk woman (as opposed to those at high risk of developing cancer), we recommend:
- Starting at age 21: A Pap test to check for cervical cancer. If the results are normal, you should be tested every three years. Pap tests are no longer recommended every year for average-risk women of any age.
- Starting at age 30: If you get a Pap test and an HPV test at the same time, and both are negative, you can move to an every-five-year testing schedule. If you only get the Pap test, you should stay on the three-year schedule.
- Starting at age 40: A yearly breast exam and mammogram to check for breast cancer.
- Starting at age 50: A colonoscopy every 10 years, a virtual colonoscopy every five years, or a fecal test (fecal occult blood test [FOBT] or fecal immunochemical test [FIT]) every year to check for colorectal cancer. If you’re African American, you should start this screening process at age 45.
Do I really need all of these screenings? Can’t I delay or put them off?
Yes, you do need them. So, no, you shouldn’t put them off. Women are less likely to die of cancer if they are screened regularly and at the ages specified. Cancer prevention experts selected the recommended starting times and intervals specifically to give doctors the best possible chance of catching cancer early, when it’s the most treatable. A woman’s risk of developing breast cancer, for instance, starts increasing at age 40, so that’s why that age was chosen.
When should I look into my family’s cancer history?
As soon as possible. Having that information available is very helpful, particularly during your first visit, because your family history can change your doctor’s screening recommendations going forward.
For instance, let’s say you’re a woman whose mother was diagnosed with breast cancer at age 45, and her mother -- your maternal grandmother -- was diagnosed with breast cancer at age 52. Because of your mother’s early age of diagnosis, we’d definitely want to talk to you about genetic testing.
We’d also consider you “high risk,” which would mean that we would start your screenings 10 years earlier than the age the youngest person in your family was when they were diagnosed with cancer. We’d probably recommend you start getting breast MRIs, too, on an alternating six-month schedule with mammograms. And we’d talk to you about preventive medications such as tamoxifen, a drug that can cut your chances of developing breast cancer in half.
Should I be tested for inheritable cancer syndromes?
Not necessarily. Genetic testing is most informative when it’s done on someone who actually has the disease. So, in the above scenario, we’d want to talk to your mother first about getting tested. If she is unavailable or unwilling to be tested, and your grandmother is no longer alive, you could be tested for genes that increase the risk of breast cancer.
The reason for this is a negative test result is not considered a “true” negative in a patient who doesn’t actually have cancer, because we haven’t identified the potential cause of the breast cancer in your family. But if your mother’s test is negative, then that is considered a “true” negative; it also means you couldn’t have inherited a genetic mutation that causes cancer from her.
Why should I come to MD Anderson for my cancer screenings?
First, because you’ll be seeing clinicians whose sole focus is cancer prevention. That is all they do -- all day, every day -- so they are the experts. When seen for evaluation, you will have your risk of developing cancer assessed, be counseled regarding a healthy lifestyle as well as other ways to reduce cancer risk (e.g., medications), and receive screening recommendations based on your individualized cancer risk.
Expertise in cancer prevention does not just apply to the clinicians you’ll see, but also to the nurses who have the knowledge to address your cancer concerns, breast imaging technologists who have unparalleled expertise to perform your mammogram, and breast radiologists who have fellowship training in interpreting images of the breast.
At MD Anderson’s Cancer Prevention Center, we see high-risk women multiple times every day; the average physician may see only a few in their entire career. And while some other hospitals do have dedicated breast imaging specialists, in most imaging facilities, the radiologist who’s looking at your mammogram is also looking at chest X-rays, back MRIs, and brain CT scans, among other things. So, they’re not specialized in looking at mammograms or other images of the breast, like our dedicated breast imagers are.
But the best reason to come to MD Anderson for cancer screenings is that we make recommendations women don’t often get elsewhere. For instance, it used to be that women had never even heard of -- much less been asked about -- genetic testing before they came to see us. It’s a bit more common now, but still not universal. Studies suggest that as many as 50% of women who should undergo genetic testing never receive a recommendation to do so. They are more likely to get this recommendation if seen at MD Anderson.
Women at increased risk of breast cancer -- whether due to a breast cancer gene mutation, a family history of the disease or a personal history of a high-risk breast lesion -- typically do not receive a recommendation from their primary care doctor for high-risk screening with breast MRI. If eligible, we commonly recommend high-risk screening with breast MRI.
Many women are also not told about medications like tamoxifen that can reduce their risk of breast cancer, which we might recommend based on their personal risk factors. We also offer our patients opportunities to participate in research studies that advance cancer science. In fact, one clinical trial is looking at the effectiveness of applying tamoxifen gel to the surface of the breast. It may or may not show the same benefit as taking that drug in pill form, but if it does, participating women are receiving cutting-edge therapy right now that may also reduce their side effects.
Therese Bevers, M.D., is medical director of MD Anderson’s Cancer Prevention Center.
Request an appointment at MD Anderson online or by calling 1-833-983-1142.

You shouldn't wait until you have a lump in your breast or blood in your stool.
Therese Bevers, M.D.
Physician