- Diseases
- Acoustic Neuroma (16)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (18)
- Bile Duct Cancer (26)
- Bladder Cancer (74)
- Brain Metastases (28)
- Brain Tumor (234)
- Breast Cancer (726)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (168)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (130)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (178)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (150)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (300)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (100)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (22)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (238)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (122)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (936)
- Research (390)
- Second Opinion (78)
- Sexuality (16)
- Side Effects (616)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (408)
- Survivorship (328)
- Symptoms (182)
- Treatment (1788)
Stages of breast cancer: How they’ve changed over time
5 minute read | Published July 05, 2022
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on July 05, 2022
In the past, only the size of a tumor and the status of nearby lymph nodes were used to determine the stage of someone’s breast cancer. It was a fairly simple system based purely on anatomy, and was therefore easy for people to memorize.
- If a tumor was two centimeters wide or smaller, it was considered stage I.
- If a tumor was larger than that or the cancer was detectable in nearby lymph nodes, it was considered stage II.
- If a tumor had spread to the skin of the breast or not far beyond the adjacent lymph nodes, it was considered stage III.
- And if a tumor had spread anywhere else in the body, it was automatically considered stage IV.
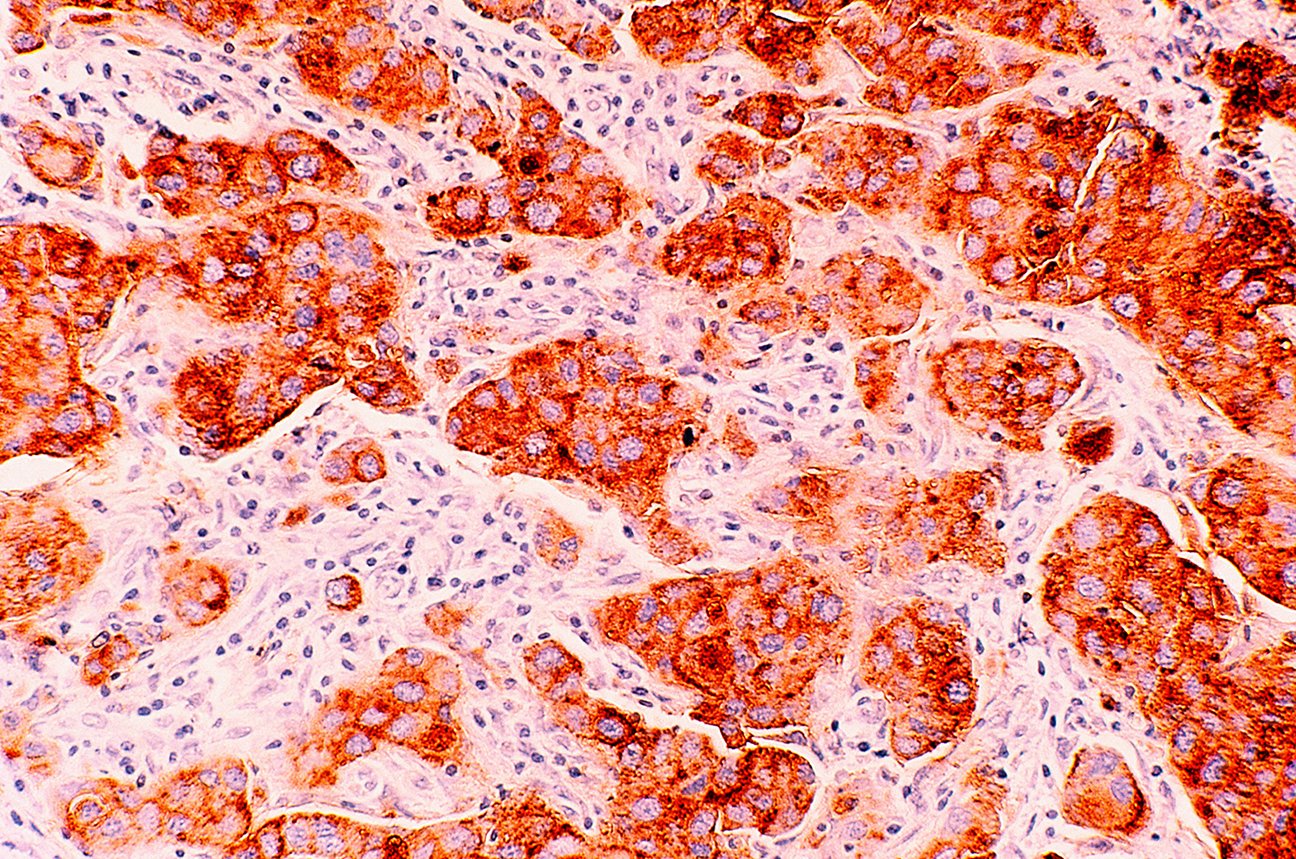
But all of that changed in 2017. Advancements in tumor biology and prognostic biological markers — such as estrogen receptor (ER), progesterone receptor (PR), and HER2/neu — allowed clinicians to understand why similarly staged patients had significantly different outcomes. This led the American Joint Commission on Cancer to revise its staging manual for breast cancer.
Today, we know that what truly determines a breast cancer’s stage is not only its size and the amount of lymph node involvement, but also what type of breast cancer it is and how aggressive it looks under a microscope.
How hormones influence breast cancer stages
Patients with hormone-sensitive breast cancers — such as ER or PR positive — now tend to be assigned lower stages when they’re diagnosed. That’s because hormone-suppressing therapies, such as anastrozole, letrozole and tamoxifen, have made them easier to treat.
So, a patient with only three cancerous lymph nodes who has a hormone-sensitive tumor that’s two centimeters wide could still be considered stage I — despite the lymph node involvement.
The presence of human epidermal growth factor receptor 2 — also known as HER2 — actually helps lower the stage, too. And that hasn’t always been the case, because HER2 positive cancer has been known to make breast cancer cells divide more quickly.
Once the targeted therapy drug trastuzumab came along, though, the prognosis of patients with HER2 positive breast cancers improved significantly. Their outlook got even better with the addition of pertuzumab. And, for patients who still don’t see a complete response from either of those targeted therapies plus chemotherapy, we can switch them to a different variation called trastuzumab emtansine.
All of these may reduce the chance of a breast cancer recurrence. And that’s pretty amazing when you think about it. Because thanks to these great new advances, having an HER2 positive cancer now can actually lower your stage.
How grades influence breast cancer stages
The grade of your breast cancer — or how different it looks under a microscope compared to normal breast cells — is also important when it comes to staging. We use something called the Nottingham scale to grade breast cancers. It has three categories.
- Grade 1: the most favorable grade; not very fast cell division and the cells look uniform and similar to normal breast cells
- Grade 2: intermediate; moderately fast cell division and the cells appear bigger and have some moderate variations in size and shape compared to normal breast cells
- Grade 3: the most aggressive grade; cells are dividing very fast and have a marked variation in size and shape compared to normal breast cells
Grades 1 and 2 often have similar stages. But Grade 3 almost always bumps you up to a higher stage, unless you have no lymph node involvement or a tumor is two centimeters wide or smaller.
Some patients get hung up on size and lymph node involvement. This is because a lot of medical facilities still use the old system. But staging is much more complex now, so what matters is not only the size and lymph node involvement, but also the type and grade of the cancer.
Why accurate breast cancer staging is important
Having your breast cancer staged accurately is critical to getting good results. That’s because staging determines your prognosis, or the goal of treatment, as well as how we treat your cancer and what treatment options are available to you.
In stages 0-3, the intent of treatment is to cure your breast cancer. But with stage IV, the goal is to manage your breast cancer — like diabetes, hypertension, or any other chronic disease — so that you can enjoy the best quality of life for as long as possible.
The addition of “a,” “b” or “c” to your stage is determined by your particular details, because the prognoses are slightly different for each one. Some patients with stage IIIc cancer are quite close to having stage IV cancer, but they still have slightly better prognoses, whether due to the presence of bulkier tumors or only having locally advanced disease. So, the details matter.
Why I am excited about the latest advances in breast cancer treatment
The good news is that there have been some really exciting advances in previously hard-to-treat breast cancers recently.
In July 2021, for instance, the Food and Drug Administration (FDA) approved the immunotherapy drug pembrolizumab for the treatment of early stage triple-negative breast cancer. And while it’s too soon to tell for sure, I do think it will lead to better outcomes for many patients.
Triple-negative breast cancers tend to be very aggressive and grow fast. But we’ve been seeing more complete responses in people who receive that drug in combination with chemotherapy. By the time we perform surgery to remove their tumors and lymph nodes, often we find there is no cancer left, and they show no evidence of disease. Only time and more data will tell us if this effect is long-lasting or not.
Right now, we’re trying to identify which markers within tumors make people more responsive to certain therapies, so we can really personalize their treatment plans. Another clinical trial called ARTEMIS, which I’m working on with lead investigator Clinton Yam, M.D., is exploring opportunities to “de-escalate” treatment plans, and see if we can achieve the same results with less therapy.
We’re also hoping to open some clinical trials through ARTEMIS that escalate therapies when people are not responding as well as we'd hoped to the current standard of care. Both of these approaches will ultimately benefit our patients.
Request an appointment at MD Anderson online or by calling 1-844-785-0306.
Related Cancerwise Stories

What matters is not only size and lymph node involvement, but also type and grade.
Oluchi Oke, M.D.
Physician