- Diseases
- Acoustic Neuroma (16)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (18)
- Bile Duct Cancer (26)
- Bladder Cancer (74)
- Brain Metastases (28)
- Brain Tumor (234)
- Breast Cancer (724)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (168)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (130)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (176)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (150)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (300)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (100)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (22)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (238)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (120)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (936)
- Research (390)
- Second Opinion (78)
- Sexuality (16)
- Side Effects (616)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (408)
- Survivorship (328)
- Symptoms (182)
- Treatment (1788)
Updates in soft tissue sarcoma
BY Andréa Bolt
5 minute read | Published June 02, 2023
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on June 02, 2023
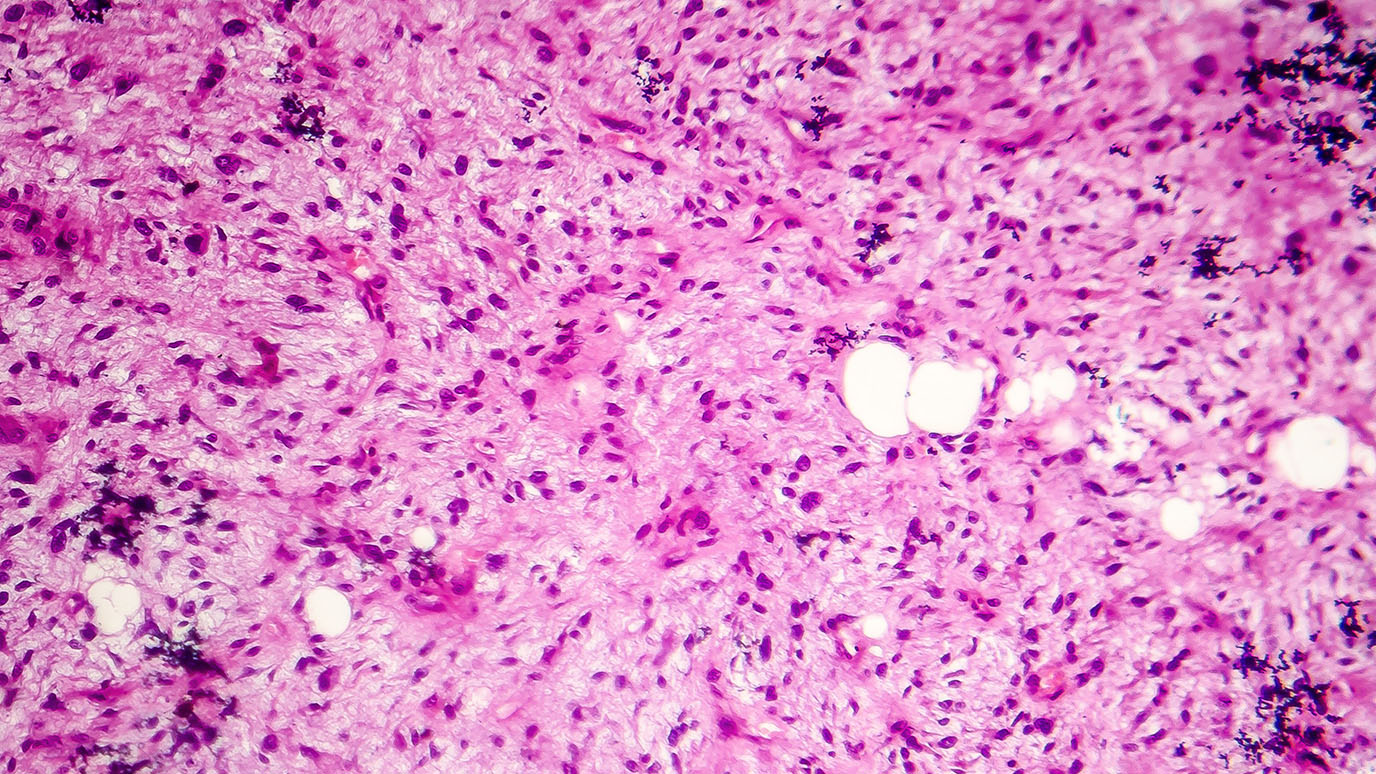
Sarcoma describes a broad group of cancers that originate in the bones and soft or connective tissues, forming in the blood vessels, nerves, muscle, fat, tendons and the lining of the joints. With over 70 types of sarcomas, treatment for this unique cancer depends on the sarcoma type, its location and a multitude of other factors.
For the latest updates in soft tissue sarcoma treatment, we spoke with Neeta Somaiah, M.D., an associate professor who is a discussant and heavily featured in presentations on the latest sarcoma research at this month’s annual American Society of Clinical Oncology (ASCO) Annual Meeting. Somaiah is proud of the research that will be presented by her colleagues and is excited to present on clinical trials concerning combination therapies. These trials show promising results regarding angiosarcoma, a sarcoma that forms in the lining of the blood vessels and lymph vessels. Liposarcomas and leiomyosarcomas are the topics of two posters.
We asked Somaiah about these recent trials and research.
There’s innovative research happening in the world of sarcoma. Tell us about the exciting sarcoma advances that you will discuss at ASCO.
At the sarcoma oral abstract session, I’ll discuss initial results from a first-in-human dose escalation trial of a novel immune-stimulating oncolytic adenovirus, AdAPT-001TGF-ß Trap will be presented by Anthony Conley, M.D., and colleagues. This novel immunotherapy approach is showing promise in some sarcoma subtypes.
Dr. Nakazawa is presenting research under the mentorship of J. Andrew Livingston, M.D., and Timothy Yap, M.B.B.S., Ph.D., looking at the loss of the DNA repair gene RNaseH2 and a unique subset of DDR-deficient leiomyosarcomas (LMS). This exciting translational biomarker work evaluating RNAseH2 loss in uterine LMS is the basis of a biomarker-selected clinical trial of ATR +/- PARP inhibition in uterine LMS that is currently under development by Dr. Nakazawa and his mentors.
Dr. Thirasastr, one of my mentees, will be presenting clinical correlations of recurring mutations in myxoid liposarcoma. These are interesting trends in chemotherapy response in myxoid liposarcoma patients. It needs further validation in a larger sample set, which could help with determining the best treatment selection for individual patients.
Your research points to success in combining therapies to treat sarcoma. Tell us about this research.
During my oral abstract session, I’ll be discussing the success of three combination trials, which concern a tyrosine kinase inhibitor called cabozantinib, which is currently gaining prominence in the sarcoma world. These clinical trial results highlight the need for optimal combination strategies based on the sarcoma subtype to help improve outcomes. Cabozantinib has been combined with immunotherapy showing high response rates and disease control in angiosarcoma patients, and cabozantinib combined with temozolomide appears to have higher response and disease control compared to what has been previously reported with either agent alone.
Tell us about the new research looking at the clinical implications of recurring mutations in myxoid liposarcoma (MLS).
Liposarcomas are the most common type of soft tissue sarcoma in adults. Myxoid liposarcomas are a subtype of liposarcoma typified by tumors that arise in the body's fat tissue, usually in the lower extremities.
Prapassorn Thirasastr, M.D., a postdoctoral fellow in Sarcoma Medical Oncology, is presenting findings from a study of recurring mutation in myxoid liposarcomas in a poster session at ASCO (abstract 11577, poster board 511). Thirasastr says he and his colleagues were generally aware that MLS is characterized by gene translocation resulting in the fusion protein, particularly involving the DDIT3 gene. Translocation means a genetic change in which a piece of one chromosome breaks off and attaches to another. Fusion proteins are created when pieces from two or more different genes join together through this chromosomal rearrangement and are then turned into a single protein. This fusion protein is considered one of the main drivers of MLS, but the exact mechanisms of how this happens are only partially understood.
However, there are two other noteworthy conclusions from the study.
One result showed that over 83% of patients tested with DNA sequencing called next-generation sequencing showed a somatic mutation, a genetic condition known to lead to cancer. Thirasastr says most of these mutations were found in the promoter region of the Telomerase reverse transcriptase (TERT) gene (TERTp), a gene involved in maintaining chromosomal stability. The recurring mutation in this hotspot was also identified in 19% of all cancers.
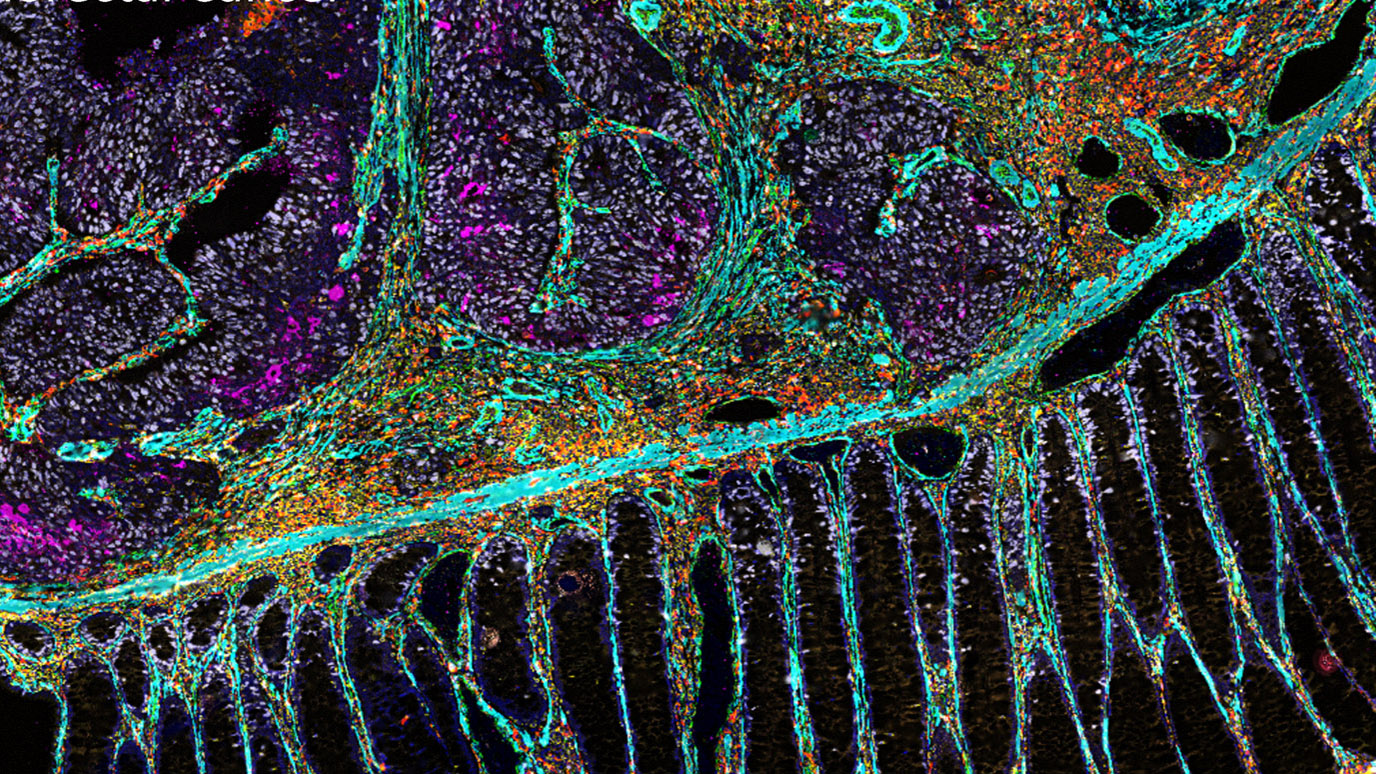
In cancer research, doctors and researchers can connect the genetic alterations in cancer cells with signaling pathways that control processes associated with the formation of tumors, which helps them piece together the signaling networks involved in fueling cancer progression.
“44% percent of MLS patients have the mutation that leads to PTEN-PI3K-AKT-mTOR pathway activation. This pathway is potentially targetable with inhibitors that are available and have been approved in other cancers,” Thirasastr explains.
Next, he said they found patients having dual mutations of PIK3CA and TERTp mutation suggests worse progression-free survival from chemotherapies.
Thirasastr says the next steps involve testing a larger population for these specific mutations to obtain larger data sets.
Another poster highlights the loss of the DNA repair gene RNase H2 and a unique subset of DDR-deficient leiomyosarcomas. Tell us about that.
Structural changes in DNA such as genetic mutations or deletions can severely interfere with its functionality, including the ability to replicate and play a significant role in both age-related diseases and cancer. Tumors that have a disruption in the DNA damage repair (DDR) gene, termed DDR-deficient, can trigger an immune response that could make them more susceptible to DNA-damaging therapies. Leiomyosarcoma, a rare cancer that grows in the smooth muscles, can occur throughout the body, including the intestines, bladder, blood vessels, skin and uterus.
Michael Nakazawa, M.D., Ph.D., a third-year Hematology and Oncology fellow who will be joining the faculty later this year, says there’s been recent interest in DDR-deficiency in leiomyosarcoma, particularly uterine leiomyosarcoma, as this general class of genetic mutations and/or deletions can sensitize tumors to targeted therapies, including PARP and ATR inhibitors. “This area is of particular interest, as currently there are no FDA-approved targeted agents for the treatment of leiomyosarcomas,” says Nakazawa, first author of a poster on this topic for ASCO (abstract 11549, poster board 483).
RNase H2 is a specific cancer-related gene not typically tested in current clinical sequencing panels. Its loss may make certain cancers susceptible to treatment with DDR-targeted therapies that are currently being tested in clinical trials.
“Our study found that RNase H2 loss is common, with up to a 30% prevalence specifically in uterine leiomyosarcoma patients, so screening could potentially broaden the number of patients who can benefit from these treatments,” says Nakazawa.
Ultimately, screening for RNase H2 deficiency may be a useful biomarker for future clinical trials of these classes of agents in uterine leiomyosarcoma patients.
Learn about research careers at MD Anderson.