- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (96)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (630)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (914)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (320)
- Symptoms (182)
- Treatment (1786)
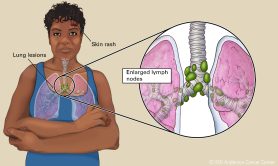
Understanding sarcoidosis: Symptoms, diagnosis and treatment
4 minute read | Published January 29, 2025
Medically Reviewed | Last reviewed by Scott Evans, M.D., on January 29, 2025
Sarcoidosis is an inflammatory disease that causes the growth of lesions called granulomas. Although it is most commonly found in the lungs, it can develop almost anywhere in the body.
We spoke with pulmonologist Scott Evans, M.D., who’s treated many cancer patients with sarcoidosis. He shares who’s at risk for sarcoidosis, why it can be tricky to diagnose and when to treat it.
Besides the lungs, where else can sarcoidosis appear?
Sarcoidosis can appear anywhere in the body. But we most often see it in the lungs; this is known as pulmonary sarcoidosis.
Sarcoidosis can also be found in the lymph nodes, skin, eyes, kidneys, thyroid gland and other organs.
What are the symptoms of sarcoidosis?
People with sarcoidosis often don’t show any symptoms.
If you do show symptoms of pulmonary sarcoidosis, they could include:
- cough
- shortness of breath
- chest pain
Sarcoidosis symptoms that affect other parts of the body may include:
- vision changes or inflammation of the eye
- rashes on the face or shins
- abnormal lab results reflecting changes in the thyroid
- changes in kidney function
Who’s at risk for getting sarcoidosis?
Sarcoidosis is an inflammatory disease triggered by an unknown cause. It can affect anyone, but some forms of sarcoidosis seem to be more common in Black women.
Historically, it was more common for people in their 30s and 40s to have sarcoidosis. In recent years, we’ve seen more cases of sarcoidosis in people in their 60s and 70s.
Why is sarcoidosis hard to diagnose?
The defining feature of sarcoidosis is an inflammatory lesion called a granuloma. Unfortunately, granuloma formation alone doesn’t tell us what the diagnosis is.
There is no single diagnostic test or pathological finding to confirm the disease. This makes it hard to diagnose sarcoidosis.
If we suspect you may have sarcoidosis based on a physical exam, you will typically get a chest X-ray or CT scan. We may also order a biopsy to sample tissue from the affected area.
It can be difficult to diagnose sarcoidosis in cancer patients
Diagnosing sarcoidosis in cancer patients presents its own challenges.
Sarcoidosis can look like other diseases. For example, imaging that shows lymphoma with enlarged lymph nodes in the chest can look very similar to sarcoidosis.
Sometimes, we can see sarcoid-like lesions around tumors. Or patients may develop lesions that look like granulomas as a side effect of certain immunotherapy drugs, such as immune checkpoint inhibitors.
So, it can be hard to rule out other diagnoses to arrive at a sarcoidosis diagnosis. Or, a biopsy could show cells that we think look sarcoidal but are not. Then we’d miss the presence of cancer cells in that biopsy.
Can sarcoidosis spread?
Yes. You can initially have sarcoidosis in the lung and later develop mucosal lesions, skin lesions or eye lesions.
When we diagnose someone with pulmonary sarcoidosis, we recommend they get evaluated to make sure they don’t have it elsewhere, like the eye or any of the endocrine organs. We don’t want to overlook other potential problems.
What triggers sarcoidosis flare-ups?
Sarcoidosis is known to spontaneously get better or worse. We don’t really know what triggers flare-ups of sarcoidosis. But we know that most people diagnosed with sarcoidosis will have spontaneous remission. That means the disease will often go away on its own.
Is sarcoidosis treatable?
Many people with sarcoidosis have very mild symptoms and do not require treatment. As many as 80% of milder sarcoidosis cases will go away on their own.
People with more advanced sarcoidosis or bothersome symptoms may need treatment.
Steroids
We usually use corticosteroids first to help reduce inflammation. They may be given as pills, creams or inhalers.
Immunosuppressants
Drugs like methotrexate, which are often used to treat some cancers, can also be used to treat sarcoidosis that doesn’t respond to steroids.
Your doctor may prescribe other treatments, depending on where the sarcoidosis is in your body.
Typically, we treat sarcoidosis the same way for people with cancer as we do for people without cancer; we don’t make modifications based on a cancer diagnosis. However, depending on the cancer treatments you’re receiving, you may not be able to take steroids. If that’s the case, speak with your doctor about the best way to manage sarcoidosis symptoms.
Treating advanced sarcoidosis
Some patients may develop persistent and progressive sarcoidosis. We usually treat these patients with higher doses of steroids or consider alternative agents, such as methotrexate.
In extremely rare cases, sarcoidosis can progress to severe lung disease. At that point, we may consider a lung transplant. Other conditions that can mimic advanced sarcoidosis include hypersensitivity pneumonitis or chronic eosinophilic pneumonia.
Monitoring sarcoidosis
If you have sarcoidosis, it’s important to see your doctor regularly to monitor the disease. If you’re on treatment, they can check to see how well it’s working and decide if they should try something else.
Remember, sarcoidosis symptoms can be vague and often mimic other conditions. Ongoing monitoring will allow your doctor to catch anything concerning right away.
Request an appointment at MD Anderson online or call 1-888-715-0014.
Related Cancerwise Stories

Many people with sarcoidosis have very mild symptoms and do not require treatment.
Scott Evans, M.D.
Physician & Researcher