- Diseases
- Acoustic Neuroma (16)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (18)
- Bile Duct Cancer (26)
- Bladder Cancer (74)
- Brain Metastases (28)
- Brain Tumor (234)
- Breast Cancer (728)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (168)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (130)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (178)
- Pancreatic Cancer (162)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
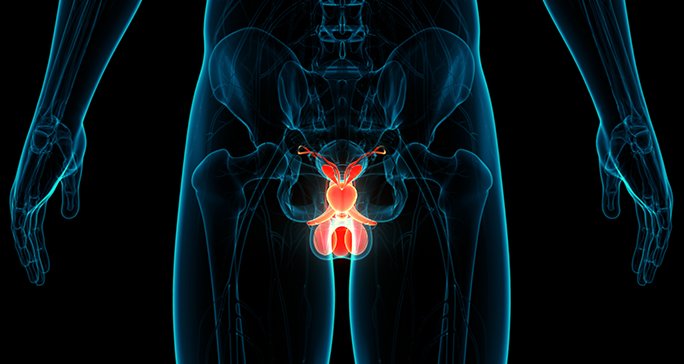
- Prostate Cancer (150)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (302)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (100)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (22)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (240)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (122)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (940)
- Research (390)
- Second Opinion (78)
- Sexuality (16)
- Side Effects (616)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (408)
- Survivorship (330)
- Symptoms (182)
- Treatment (1794)
Renal medullary carcinoma: 5 things to know about this rare and aggressive kidney cancer
5 minute read | Published September 03, 2024
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on September 03, 2024
Renal medullary carcinoma (RMC) is a rare and extremely aggressive kidney cancer. In the United States, it is diagnosed most frequently among young Black men who carry the sickle cell trait, an inherited blood mutation.
But do you have to carry the sickle cell trait to develop renal medullary carcinoma? How else does it differ from other kidney cancers? And, what are the latest advances in its diagnosis and treatment?
Here, medical oncologist Pavlos Msaouel, M.D., Ph.D., answers these and other questions about renal medullary carcinoma.
Do you have to carry the sickle cell trait to be at risk for renal medullary carcinoma?
No. Most people who are diagnosed with it will carry the mutation, but between 5% and 10% of all renal medullary carcinoma cases are not associated with that trait.
How does renal medullary cancer differ from other kidney cancers?
The biggest difference is in its treatment. Almost every single strategy developed for garden variety kidney cancer does not work with renal medullary carcinoma. In fact, they often make it worse.
With most early-stage kidney cancers, for instance, you can start with surgery, if a tumor is small enough. But in most renal medullary carcinoma cases, you need to start with chemotherapy.
That’s because most kidney cancers do not spread to the lymph nodes nearly as much as renal medullary carcinoma does. Renal medullary carcinoma loves to spread to lymph nodes, and it does so at a much higher rate than any other kidney cancer.
So, even if imaging isn’t showing renal medullary carcinoma in your lymph nodes, it’s probably there if you have it in your kidney. But a surgeon will typically only discover that after the fact. Also, we can’t know if chemotherapy is working unless we can track a tumor’s response to it over time on imaging. That’s why it’s so important to start treatment for RMC with chemotherapy first.
Finally, the right kidney tends to be more susceptible to renal medullary carcinoma than the left. We believe this is because the artery that supplies the right kidney is longer, so it takes more time for the blood to get there. There’s also more resistance with a longer tube, so there’s less blood flow in the right kidney's artery. That makes it more prone to infarcts, or tissue damage caused by a lack of oxygen.
Are the symptoms of renal medullary carcinoma any different from those of other kidney cancers?
No, not really. Hematuria, or blood in the urine, is the most common symptom of renal medullary carcinoma. But it can also be a symptom of all kidney cancers. We see it in about 60% of our renal medullary carcinoma patients here at MD Anderson.
Pain is the second-most common symptom. We see it in a little less than half of all renal medullary carcinoma cases. Again, pain can be a symptom of all kidney cancers. In RMC, it’s usually on the side that has the cancer, most often on the right.
Less common symptoms include belly pain and weight loss. But those only happen in about 20% of our patients with renal medullary carcinoma.
Why should people choose MD Anderson for their renal medullary carcinoma treatment?
Renal medullary carcinoma is very, very rare, so most clinicians will only see one case of it in their entire careers, if that. But my mentor, genitourinary medical oncologist Nizar Tannir, M.D., started building our program more than a decade ago, after a patient of his died of the disease. That program, which I now lead, has a lab that works exclusively on renal medullary carcinoma.
I’d also estimate that I personally help manage more than 80% of all renal medullary carcinoma cases in the world. Doctors reach out to me from as far away as New Zealand, Germany, Greece and Norway for guidance, and I’m always happy to provide it.
Another reason to choose MD Anderson is that, with treatment, we render up to 10% of our patients with stage IV renal medullary carcinoma cancer-free, which was thought to be impossible five years ago. MD Anderson was also the first to design a clinical trial just for renal medullary carcinoma and the first to get any funding for its research.
We’ve increased the average length of survival after a renal medullary carcinoma diagnosis, too. Back when it was first described in 1995, patients typically only survived about four months after their diagnosis. By 2017, the average survival had improved to 13 months. But research has really accelerated since 2018, and now it’s at least 18 months. Our goal is to extend that to two years by 2025, and to five years by 2030. We’re on pace to get there.
What are the most exciting advances in renal medullary carcinoma research?
We’ve always got at least one clinical trial available for renal medullary carcinoma patients. But our latest, which opened Sept. 1, is designed to harness the immune system in a better way to target CA-125, a chemical marker normally seen in ovarian cancer. My lab discovered that it’s also expressed by renal medullary carcinoma. Another rare cancer called epithelioid sarcoma, which has the same molecular driver as renal medullary carcinoma, also expresses CA-125.
Until 2012, we only had one standard therapy for RMC: carboplatin plus paclitaxel. Then, we established a second-line therapy that used gemcitabine and doxorubicin, either alone or in combination with ixazomib. Later, we established a third-line therapy that targets the EFGR pathway with panitumumab, carboplatin and nab-paclitaxel. And now, we have clues for a fourth-line therapy that targets the TROP2 pathway.
In May 2022, I was reviewing some experiments in my lab and started noticing certain patterns. I discussed them with my wife, who is a breast medical oncologist here at MD Anderson, and she had the idea to try a targeted therapy against the EGFR pathway first used to treat breast cancer. Within a week, we had repurposed that therapy for a patient with stage IV renal medullary carcinoma, and he’s still responding well to it today. Since that time, this combination of panitumumab, carboplatin and nab-paclitaxel has been given to more than 20 people with renal medullary carcinoma around the world.
Request an appointment at MD Anderson online or call 1-833-777-0195.
Related Cancerwise Stories

The right kidney tends to be more susceptible than the left.
Pavlos Msaouel, M.D., Ph.D.
Physician & Researcher