- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (96)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (630)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (914)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (320)
- Symptoms (182)
- Treatment (1786)
Rectal cancer surgery: Your treatment options and what to expect
5 minute read | Published January 11, 2023
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on January 11, 2023
Rectal cancer can impact many of the body’s most basic functions. So, it’s important to find a surgeon who understands the balance between treating your cancer and preserving the body's functions and quality of life.
To learn about the different types of rectal surgery and what to expect, we spoke with Yi-Qian Nancy You, M.D., a colon and rectal cancer surgeon.
What types of surgery are used to treat rectal cancer?
There are three types of surgery used to treat rectal cancer.
- Transanal local excision: This procedure treats very early-stage rectal cancers. During this procedure, a surgeon removes a small area of the rectum wall that contains the early tumor through instruments that are passed through the anus.
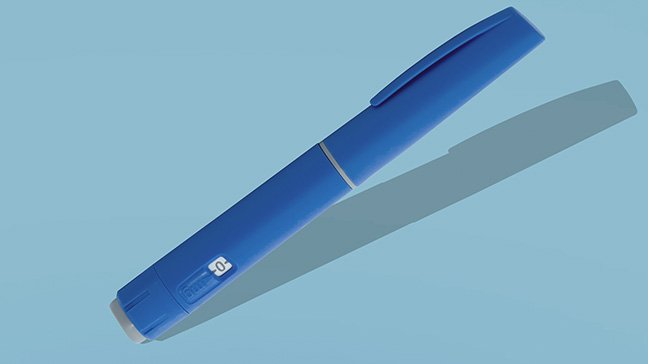
- Proctectomy: During this surgery, a surgeon removes all or part of the rectum that contains the tumor. Usually, the colon can be brought down and connected to the remaining rectum or directly to the anus in sphincter-preserving surgery. This allows the patient to retain bowel passage through the anus, although the stool frequency and patterns will likely be different. Often to protect the new connection, the surgeon will make a temporary diverting ileostomy bag, a plastic bag that collects waste from the digestive tract and needs to be emptied throughout the day. This is done to divert the stool away from the colon and give the new connection the best chance to heal. If the sphincter can’t be preserved, the surgeon will create a permanent colostomy and insert a colostomy bag, a plastic bag that collects waste from the digestive tract and needs to be emptied throughout the day.
- Pelvic exenteration: This type of surgery is needed if rectal cancer has spread to the surrounding organs within the pelvis. During this highly specialized operation, surgeons will remove the rectum containing the tumor and any part of any adjacent organs that may be also directly involved by the tumor — including other bowel or intestine, reproductive organs, bladder, bone or other tissue — and then perform the reconstruction. Patients who have had a pelvic exenteration often need a colostomy bag.
What is recovery from rectal cancer surgery like? What can patients expect?
Your recovery depends on what type of surgery you undergo. Patients who have a proctectomy typically stay in the hospital for two to five days, or they may have to stay until they have a bowel movement. Patients are usually up and walking around about 24 hours after surgery. Typically, bowel function will return about two to three days following surgery. Pain is the strongest for the first 48 hours and then begins to subside. MD Anderson surgery teams rely on an enhanced recovery process that helps patients recover faster and limit their use of pain medication.
For patients who have undergone a pelvic exenteration, the recovery process is slower. Typically, these patients stay in the hospital for two to three weeks and spend the following months getting their strength back by working with a physical therapist.
Patients who have had a temporary ileostomy or permanent colostomy as a part of their proctectomy or pelvic exenteration may need to stay in the hospital longer as they adjust to using the ostomy bag.
What is life like after rectal cancer surgery? Do patients with an ileostomy or colostomy bag need to make dietary changes?
An ostomy bag may be temporary. Patients may only need it for two to six months, or it may be permanent. Your care team will work with you to show you how to empty the bag and make any other changes. Having an ostomy will require some adjustment and adaptation. However, most importantly, contrary to common belief, patients with ostomy bags can resume an active lifestyle and get back to activities they enjoyed before surgery.
Read how one young patient has learned to live with her ostomy bag.
What other methods are used to treat rectal cancer?
Many rectal cancer patients will need additional treatments, typically a combination of chemotherapy and radiation and typically before surgery. For rectal cancer, it’s important to see a specialized care team with experience treating rectal cancer and who understand all aspects of your rectal cancer treatment. When you’re choosing a care team, look for one that will coordinate your care and enable you to receive the best treatment possible.
Overall, the cancer stage determines the type of treatments a rectal cancer patient received. But an experienced team also takes into account the patient’s tumor molecular characteristics and personal wishes to design a personalized treatment regimen. In addition, MD Anderson is conducting clinical trials to use liquid biopsies to more accurately determine what next steps to take. The biopsies show how cancer has impacted the bloodstream and helps guide the use of chemotherapy after surgery.
1 in 4 new cases of rectal cancer in the U.S. is diagnosed at or under age 50. What should young rectal cancer patients know?
Young rectal cancer patients face a unique set of challenges. They have so many years left ahead of them, but they’re facing big changes as survivors. For these patients, it’s particularly important to select a cancer center like MD Anderson where the doctors are not only experts in treating rectal cancer, but also understand what’s critical to a young patient. At MD Anderson, one-third of all of our new colorectal cancer patients are younger than age 50. Programs like MD Anderson’s Young-Onset Colorectal Cancer Program provide cancer care and connect patients to services they may need in addition to treatment, including genetic testing and counseling, fertility services, wound ostomy service, supportive care and connection to our Adolescent and Young Adult Oncology Program.
What should patients preparing for rectal cancer surgery know?
Look for a care team where the surgeons both perform a high number of rectal cancer surgeries and are also experts in treating rectal cancer and in understanding the best coordination of surgery with other treatments, such as chemotherapy and radiation.
Rectal cancer impacts an area that is key to many bodily functions, so it’s essential to seek a care team that truly understands it and with whom you feel comfortable discussing your worries and concerns.
Often, we see patients who first underwent surgery at another hospital. In many cases, the patient’s cancer has returned and they now need a pelvic exenteration. While MD Anderson surgeons are skilled at performing this complicated surgery, it would be easier on the patient if they sought care from leading experts first. It might be difficult to decide to have more of the rectum removed initially, but it’s better in the long run. At MD Anderson, our doctors understand how to balance this.
Request an appointment at MD Anderson online or by calling 1-855-701-7200.

Look for a care team where the surgeons both perform a high number of rectal cancer surgeries.
Yi-Qian Nancy You, M.D.
Physician