- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (294)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (96)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (630)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (912)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (320)
- Symptoms (182)
- Treatment (1786)
Q&A: Choosing the Best Prostate Cancer Treatment
BY MD Anderson
4 minute read | Published September 06, 2011
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on September 06, 2011
Due to the multiple treatment choices available for men with prostate cancer, MD Anderson physicians in the Genitourinary Cancer Center formed the Multidisciplinary Prostate Cancer Clinic in 2004. Their aim is to help men choose the best treatment options for their cancer.
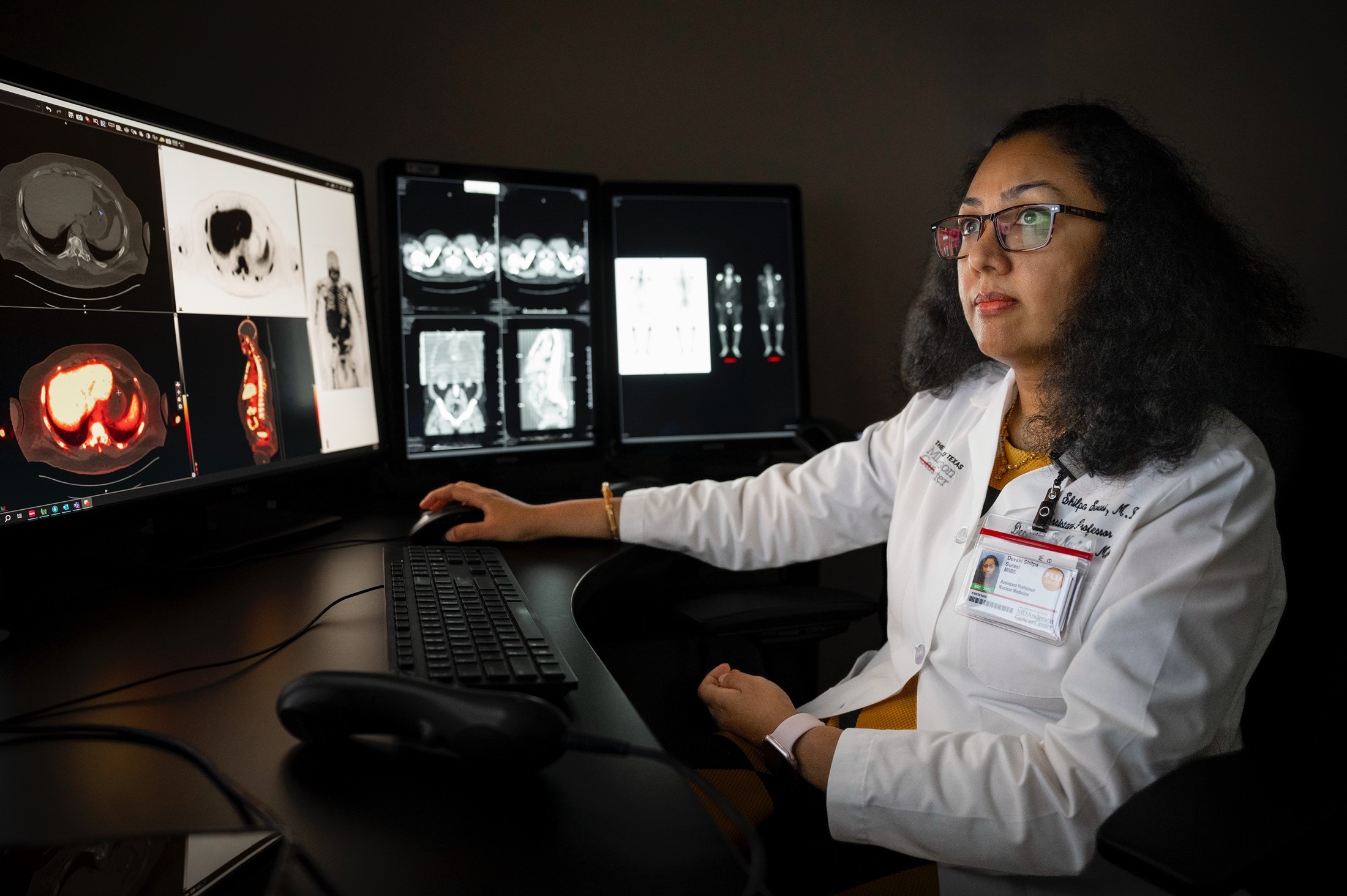
Deborah Kuban, M.D., professor in MD Anderson's Department of Radiation Oncology, answers questions regarding the clinic and prostate cancer treatment options.
Why was the clinic created?
For prostate cancer, there are many treatment options available. Along with this, physicians can be inherently biased toward the type of treatment they provide.
We wanted patients to get a very well-rounded opinion on all treatment options available to them. This would allow them to be active in the decision-making process.
Recent conclusions from urologists and radiation oncologists -- the two main physicians who treat early prostate cancer -- are that there is no one best treatment option for prostate cancer patients.
Sometimes we see patients who don't want options. They want a decision.
When this happens, we have to explain that we can't always tell them what to do because that would be biased. For some, there are multiple options that would produce equally good outcomes. We can't just arbitrarily say whether they should have radiation or surgery when both are equally good.
We also tailor our recommendations around each patient's needs regarding their cancer, other medical problems and social situation.
We also take into consideration quality-of-life issues and whether a patient would be more bothered by one particular side effect over another. It's well known that incontinence is more likely to occur after surgery, and that radiation may cause problems with bowel function. Both carry significant risk of impotence.
We try to look at the whole picture. Not just the cancer characteristics.
Why does a patient come to the clinic?
Patients often come to the clinic to make a decision about their primary treatment. The typical patient is newly diagnosed with prostate cancer and is unsure of how he wants to be treated.
The sequence of events that usually leads a patient to the clinic begins with his urologist identifying an elevated prostate specific antigen (PSA) level in his blood work or something suspicious during a rectal exam. Both typically prompt a biopsy of the prostate to determine if it's cancerous.
If a patient has already seen several physicians for treatment options and is determined to follow through with one, he won't visit the clinic. We refer him directly to the appropriate physician.
What takes place during a clinic appointment?
When the patient arrives, he's met by our advanced practice nurse Lydia Madsen. She outlines the schedule for the day and whom the patient will see -- a urologist and radiation oncologist. For more advanced prostate cancer, a patient also sees a medical oncologist.
The physicians review the patient's medical history before examining and speaking with him. After the consultations, the physicians give a consensus statement on what treatment options are recommended. The options are also provided to the patient in a letter.
Madsen is also the last person the patient sees before he leaves. She goes over all the treatment options with him. If one is chosen, the patient is scheduled for it. He then receives a treatment map, which lays out all the steps he will take to complete the treatment process. If he wants to take time to think about it, he's able to call Madsen later with a decision.
What treatment options are available?
Standard treatments for prostate cancer include:
- Radiation treatment
- Surgery
- Active surveillance
- Medical treatment
There are two forms of radiation treatment, external and internal. External radiation includes external beam (X-ray) radiation and proton beam therapy. Intensity-modulated radiation therapy (IMRT) is often referred to, and this is the latest technique for external beam therapy.
External beam radiation can be more widely applied to patients since tumor stage, prostate size and urinary function are not such critical considerations. Internal radiation is referred to as brachytherapy or seed implant. With this technique small seeds of radiation are implanted directly into the prostate and deliver a constant dose.
Prostatectomy is surgical removal of the prostate. There are two main techniques: open and robotic assisted, and each has pros and cons. Patients who have other significant health problems, are over 70 years old or who may have problems with anesthesia generally consider options other than surgery.
Active surveillance may be recommended for older patients with limited life span and for those with very early cancer that may not become problematic for many years. It's also called "watchful waiting" because no treatment is given, but the patient is monitored closely by a physician. This option can be used for the patient's lifetime or for a period of time before a treatment option is pursued.
Medical treatment encompasses hormone therapies, which affects testosterone and inhibit the proliferation of the cancer, as well as chemotherapy, which is generally used in late stages. Hormone therapy is usually only used for prostate cancer that has spread outside the prostate or when the patient is elderly or ill.
The opportunity to participate in clinical trials is also an option for appropriate patients.
How can patients access the clinic?
Patients can self-refer or their physician can refer them for an appointment.
Related stories
With Faith, Family and a Plan, Man Beats Prostate Cancer