- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (722)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (176)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (148)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (298)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (236)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (928)
- Research (388)
- Second Opinion (76)
- Sexuality (16)
- Side Effects (614)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (324)
- Symptoms (182)
- Treatment (1778)
Pivotal moment shapes physician’s patient-centered care
BY Katie Brooks
2 minute read | Published January 03, 2024
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on January 03, 2024
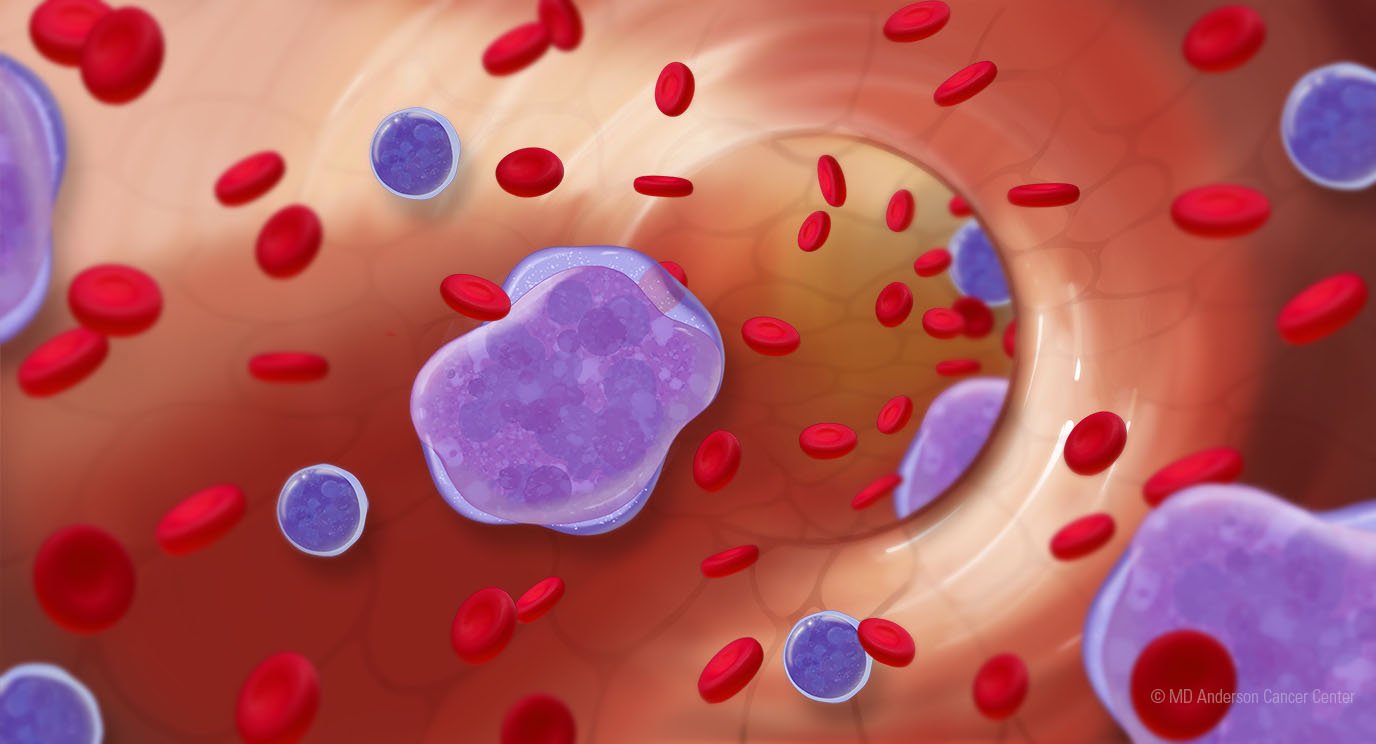
While she was a physician in training in Chicago, Sairah Ahmed, M.D., was struck by the similarities between her and a young leukemia patient. Both were intelligent, goal-oriented American women of south Asian descent. They were even the same age. They met and got to know each other throughout the patient’s chemotherapy, hospital stays and toxicity checks.
“She was the only child. Beloved by her parents, aunts, uncles and entire family,” Ahmed says, recalling the patient who made a profound impact on her when she was just a fellow. “She was their world.”
Precious time, spent the patient’s way
When the woman’s cancer relapsed, Ahmed talked with her about next steps. Ahmed remembers a conversation they had in the ICU in which the woman confided that she did not want to die in the hospital.
“She didn’t want to add to her parents’ pain by telling them she was ready to go home,” Ahmed recalls. “She knew they wanted more treatments for her. I talked to her parents about what she wanted and started the conversation for her.”
The patient decided to go home and was there for a while, before returning to the hospital, where she eventually passed away.
“Her mom, dad, aunts and uncles thanked me for talking to them,” Ahmed says. “They appreciated the time they had at home with their daughter, saying they were some of her best days.”
Because of that experience, Ahmed builds relationships with each of her patients at MD Anderson by having open and honest conversations about what’s important to them and advocating to ensure their care supports their priorities.
Patients’ priorities come first
Ahmed, an associate professor in Lymphoma/Myeloma, has goal concordant care conversations early in her patients’ care, and often, because things change.
Whether it’s about preserving their fertility, continuing their favorite activities or setting aside time to make memories, talking through things gets the patient, their loved ones and their care team members on the same page so they can move forward to the next step together, she says.
Goal concordant care is holding and documenting conversations about what matters most to patients throughout their care.
“Having cancer can mean feeling betrayed by your body,” Ahmed says. “When patients have their needs heard, and prioritized, it restores a small sense of control. We can do right by each patient by making sure we are asking about and being respectful of their individual priorities.”
She’s proud of the progress MD Anderson teams have made with communication skills training, new tools and process improvement.
The most rewarding part? What her patients tell her.
“They are vocal about appreciating these conversations,” she says. “They trust they will get honest answers so we can make decisions together on what’s best for them no matter what.”
Request an appointment at MD Anderson online or call 1-833-531-0983.
Related Cancerwise Stories

When patients have their needs heard, and prioritized, it restores a small sense of control.
Sairah Ahmed, M.D.
Physician