- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (66)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (28)
- Bladder Cancer (68)
- Brain Metastases (28)
- Brain Tumor (228)
- Breast Cancer (716)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (154)
- Colon Cancer (164)
- Colorectal Cancer (110)
- Endocrine Tumor (4)
- Esophageal Cancer (42)
- Eye Cancer (36)
- Fallopian Tube Cancer (6)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (6)
- Kidney Cancer (124)
- Leukemia (344)
- Liver Cancer (50)
- Lung Cancer (288)
- Lymphoma (284)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (98)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (170)
- Pancreatic Cancer (166)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (144)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (236)
- Skin Cancer (294)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (60)
- Testicular Cancer (28)
- Throat Cancer (90)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (78)
- Vaginal Cancer (14)
- Vulvar Cancer (18)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (624)
- Complementary Integrative Medicine (24)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (230)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (122)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (892)
- Research (390)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (602)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (404)
- Survivorship (322)
- Symptoms (184)
- Treatment (1770)
Peripheral neuropathy in cancer patients
4 minute read | Published June 18, 2014
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on June 18, 2014
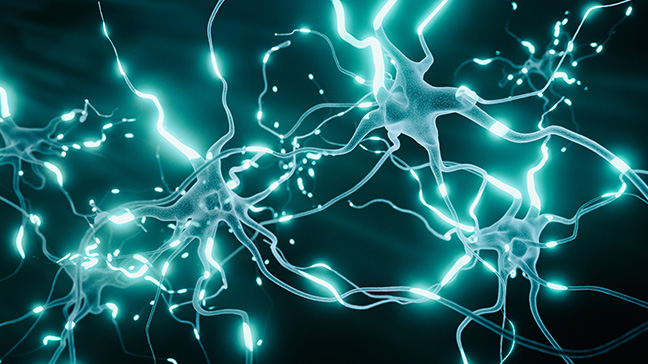
For many of our patients, peripheral neuropathy is among the unexpected side effects of cancer treatment.
It's caused by damage to your peripheral nerves -- that is, the nerves that are farther away from your brain and spinal cord. Certain complications of cancer or cancer treatments can cause or worsen neuropathy. So can some health conditions, such as diabetes, alcoholism, AIDS, hypothyroidism, rheumatoid arthritis and carpel tunnel syndrome.
We recently spoke with Julie Walker, advanced practice nurse in Neuro-Oncology, about peripheral neuropathy. Here's what she had to say.
What causes peripheral neuropathy in cancer patients?
The nerve damage that causes peripheral neuropathy may be the result of many different factors, including some chemotherapy drugs using vinca alkaloids, platinum compounds, taxanes and thalidomide.
Tumors themselves can cause nerve damage as well if they grow close to and press on the nerve.
And, patients with cancers of the nervous system -- such as brain tumors, spine tumors and skill base tumors -- are more likely to develop peripheral neuropathy due to nerve damage resulting from the tumor.
What are common peripheral neuropathy symptoms?
Symptoms depend on the type(s) and location(s) of the damaged nerves. The most common peripheral neuropathy symptoms include:
- numbness
- tingling
- shooting pain or burning, especially in your fingers or toes.
Other peripheral neuropathy symptoms include:
- loss of balance, difficulty walking or frequent falls
- clumsiness
- difficulty picking up objects or buttoning your clothes
- facial pain
- hearing loss
- loss of sensitivity to hot and cold
- stomach pain
- constipation
What can cancer patients do to relieve peripheral neuropathy?
If the neuropathy is related to something you can control, try to control the cause.
If your neuropathy is chemo-related, your oncologist can decide whether it's beneficial to reduce your chemotherapy dosage or switch to a different treatment regimen.
If it's related to diabetes, you can often slow down or stop the progression of peripheral neuropathy with better blood sugar control.
Beyond that, physical activity can help by keeping blood flowing in the affected areas. Some people also try acupuncture.
Over-the-counter pain relievers and prescription medications like carbamazepine and Lyrica may help in some cases. Non-prescription-type treatments -- such as acetyl l-carnitine, alpha lipoic acid, glutamin, calcium and magnesium -- may help, too. But more research is needed to better gauge their effectiveness. Be sure to speak with your health care provider before trying any of these.
What can cancer patients do to lower their chances of developing peripheral neuropathy?
If you have other health conditions, such as diabetes, that can make the neuropathy worse, manage them appropriately. Limit alcohol use. Maintain a well-balanced diet. And, discuss your neuropathy risks with your health care provider.
How long do peripheral neuropathy symptoms last?
Every case is different. Because neuropathy is caused by nerve damage, it depends largely on how well your nerves recover. And, that depends on the length of your treatment, extent of the damage and, in the case of chemotherapy-induced neuropathy, dosage intensity.
It's usually possible to manage peripheral neuropathy up to a certain point, but for many people, it never goes away.
As the nerves heal, some people may actually experience more tingling in the affected area. Speak with your health care provider to find out if a prescription might help relieve symptoms during this time.
People with peripheral neuropathy lose the ability to feel pain or extreme temperatures in the affected areas.
What can cancer patients with peripheral neuropathy do to avoid burning or injuring themselves?
Always wear shoes to protect your feet from an injury. Also, make sure you examine your feet every day to look for any wounds or sores that aren't healing.
Be careful when using sharp utensils or avoid them altogether. Likewise, since neuropathy typically inhibits your fine motor movements, be cautious around or avoid dangerous machinery.
Before touching water with your hands or feet, feel the water with a part of your body -- such as the underside of your forearm -- that can sense how warm it is. And, avoid using heating pads and hot water bottles.
Any other advice for cancer patients who are experiencing neuropathy?
People with neuropathy are more prone to falls because they struggle to feel the ground beneath them, especially in the dark or an enclosed space. So:
- use a nightlight
- keep clutter and throw rugs off the floor
- use handrails when taking the stairs
- put handrails in the shower
- use skid-free shower and bath mats
Neuropathy also makes the body more prone to infection since circulation is decreased and wounds don't heal as well. So it's a good idea to keep your skin moist to prevent cracking and, in turn, infection.
The most important thing you can do, though, is to speak with your health care provider as soon as you start to experience neuropathy symptoms. Together, you can hopefully find ways to manage your symptoms.