- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (66)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (28)
- Bladder Cancer (68)
- Brain Metastases (28)
- Brain Tumor (230)
- Breast Cancer (716)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (154)
- Colon Cancer (164)
- Colorectal Cancer (110)
- Endocrine Tumor (4)
- Esophageal Cancer (42)
- Eye Cancer (36)
- Fallopian Tube Cancer (6)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (6)
- Kidney Cancer (124)
- Leukemia (344)
- Liver Cancer (50)
- Lung Cancer (288)
- Lymphoma (284)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (98)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (170)
- Pancreatic Cancer (166)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (144)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (236)
- Skin Cancer (294)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (60)
- Testicular Cancer (28)
- Throat Cancer (90)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (78)
- Vaginal Cancer (14)
- Vulvar Cancer (18)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (624)
- Complementary Integrative Medicine (24)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (230)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (122)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (892)
- Research (390)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (404)
- Survivorship (322)
- Symptoms (184)
- Treatment (1772)
New research offers treatment advances for stomach and esophageal cancers
5 minute read | Published January 26, 2021
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on January 26, 2021
Stomach and esophageal cancers are diagnosed in more than 40,000 people each year in the U.S. Most of these cases aren’t detected until the cancers are advanced. Unfortunately, available treatment options are not as effective once a cancer becomes metastatic.
Most patients with metastatic stomach or esophageal cancer are treated with combination chemotherapy, but their outcomes can vary widely.
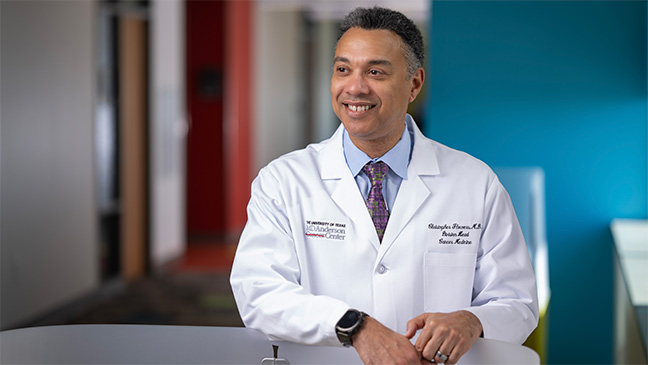
“We select combinations based on what has worked for most patients in the past. However, we can’t know in advance how a cancer will respond to therapy, or whether the patient will benefit long-term or not at all,” says Jaffer Ajani, M.D. “We have a real need to better understand the basic biology of this disease so we can tailor therapies to each patient and identify new treatment strategies.”
Ajani worked with MD Anderson colleagues to answer these questions. Two of their studies were recently published in the journal Gut.
Genetic study finds factors linked with patient survival and new therapeutic targets
Biomarkers can help physicians predict how patients will respond to therapy. This insight can be valuable for guiding treatment plans, identifying patients who may benefit from minimal therapy and those who may have an aggressive disease. However, these effective biomarkers haven’t yet been identified for stomach and esophageal cancers.
To fill this void and better understand why patients respond differently to treatment, a research team, led by Dapeng Hao, Ph.D. and Ajani, conducted an in-depth study of metastatic stomach and esophageal cancers.
The researchers performed genetic analyses on tumor samples from 20 patients who had typical responses and 20 patients with exceptional responses to treatment. While there were many similarities, the researchers discovered a number of notable differences.
They found a greater degree of tumor diversity in the patients who did not respond well. Mutations in the KMT2C gene were present exclusively in this group.
The tumors in these patients also frequently had a portion of chromosome 4 missing, a phenomenon associated with poor outcomes in many cancer types. Looking more closely, the researchers found that losing chromosome 4 resulted in a “cold” immune environment. This means the immune system could not mount a strong response against the tumor.
On the other hand, exceptional responders in this study tended to have different sets of gene mutations related to the activity of a protein called APOBEC. These mutations, which could be seen as abnormal by the immune system, are thought to lead to a stronger anti-tumor immune response.
Taking all of their findings together, the researchers developed a new model to help predict patient outcomes using genetic information and clinical factors. This new tool may be useful in identifying patients who are likely to respond well to treatment and those who may need more aggressive treatments.
“Our integrated model, if validated in clinical studies, can help predict how a patient will respond to before they ever begin treatment. If a patient falls in one group, they may benefit from immunotherapy approaches, while patients in the other group may need different strategies,” says Hao. “This research also pointed to important biological insights, including possible new treatment targets in these cancers.”
New targeted therapy shows early promise for advanced stomach and esophageal cancers
Advanced stomach and esophageal cancers frequently develop resistance to available therapies and stop responding. Each additional line of treatment tends to be less effective, Ajani explains. This can make treating them a challenge.
Therapy resistance is thought to be driven by a small number of “cancer stem cells.” Standard chemotherapies don’t specifically target these cells, so they tend to survive and allow the cancer to regenerate itself over time, leading to relapse.
MD Anderson researchers, led by Shumei Song, M.D., Ph.D., and Ajani, studied an experimental targeted therapy, called AT101, to determine if it could effectively kill cancer stem cells in stomach or esophageal cancer.
By studying stomach and esophageal cancer cells in the laboratory, the researchers found that they had increased levels of the Mcl-1 and Bcl-2 proteins, which normally act to prevent programmed cell death. These proteins were also found at higher levels in tumor samples compared to normal tissue.
The researchers, therefore, tested AT101, which is designed to block Mcl-1 and Bcl-2 activity, in cancer cells. The drug appeared to effectively block Mcl-1/Bcl-2 and stop the growth of cancer cells. The drug also blocked pathways known to be important in cancer stem cells and was effective in killing these cells in particular.
In preclinical models, combining AT101 with docetaxel, a chemotherapy commonly used to treat these cancers, dramatically reduced tumor growth. Adding radiation therapy to the combination was even more effective.
Based on these encouraging preclinical studies, the researchers led a Phase I clinical trial of AT101 in combination with chemotherapy and radiation therapy. Of the 13 patients enrolled on the study, 11 had a complete response, meaning there was no evidence of disease after treatment. Ten patients eventually had a recurrence, with a median progression-free survival of one year.
The most common side effects were gastrointestinal issues, including vomiting, loss of appetite and painful swallowing. A total of nine serious adverse events occurred, including one death on the trial, although these were not considered to be related to the therapy. Treatment was temporarily paused in three patients because of elevated protein levels, and two patients were eventually able to continue therapy.
“We are encouraged by the promising early activity of our combination treatment strategy, which seems to work synergistically against both the bulk of the tumor and the cancer stem cells,” says Song. “We hope to continue evaluating AT101 or similar drugs and other combination therapies to bring more effective treatment options to patients with advanced stomach or esophageal cancers.”
Refer a patient to MD Anderson online or by calling 1-855-781-4421.
Related Cancerwise Stories

We have a real need to better understand the basic biology of this disease so we can tailor therapies to each patient and identify new treatment strategies when needed.
Jaffer Ajani, M.D.
Physician & Researcher