- Diseases
- Acoustic Neuroma (16)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (18)
- Bile Duct Cancer (26)
- Bladder Cancer (74)
- Brain Metastases (28)
- Brain Tumor (234)
- Breast Cancer (726)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (168)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (130)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (178)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (150)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (300)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (100)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (22)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (238)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (122)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (936)
- Research (390)
- Second Opinion (78)
- Sexuality (16)
- Side Effects (616)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (408)
- Survivorship (328)
- Symptoms (182)
- Treatment (1788)
Neurodegeneration and cancer: What’s the link?
BY Julie Nagy
4 minute read | Published November 28, 2023
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on November 28, 2023
Recent studies have shown that age-related neurodegenerative diseases such as Alzheimer’s disease and Parkinson’s disease occur less frequently in cancer survivors, but little is known about the role of the nervous system in cancer progression.
We spoke to Moran Amit, M.D., Ph.D., assistant professor of Head and Neck Surgery, to help clarify this potential link and to learn about the work his lab is doing to help further our understanding of cancer neuroscience, a rapidly emerging field that combines many aspects of cancer biology, aging, immunology and neurobiology.
What is neurodegeneration?
The term ‘neurodegeneration’ refers to the progressive damage, or degeneration, of nerve cells. This can be applied to several diseases that involve neuronal loss and function and can result in the breakdown of things like memory and decision-making.
As people age, the brain and nervous system go through natural breakdowns, and sometimes waste products and other chemicals can collect in the brain tissue. This often leads to plaques, inflammation, tangles and fatty buildup that are associated with neurodegenerative diseases.
How is the nervous system linked to cancer?
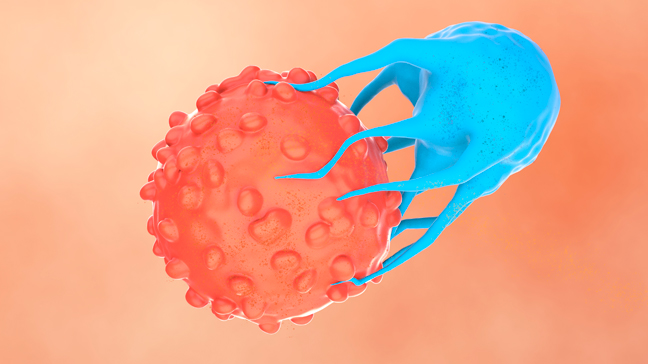
The nervous system is involved in many functions of the human body. It is important to recognize and advance our understanding of its contribution to cancer, including neural signaling interactions that regulate tumor growth, metastasis, treatment resistance and inflammation, so we can identify therapeutic targets and improve treatments.
Nerves are protected by a myelin sheath, an insulating layer made up of protein and fatty substances that allow electric signals to transmit quickly and smoothly along nerve cells. When this myelin sheath gets damaged, it causes electric impulses to slow down, contributing to symptoms of neurodegeneration such as cognitive decline and memory loss.
When looking at population-level data, we see that neurodegeneration in the forms of Alzheimer’s disease or other types of dementia is conversely associated with cancer. This means you see more cancer in patients who have less cognitive decline and vice versa. Interestingly, when we induce neurodegeneration in tumors by demyelination, we see that many of those nerves express markers for Parkinson’s, Alzheimer’s and Lou Gehrig’s disease.
Our lab has also found markers of neural degeneration in the peripheral nervous system, the nerves that branch out from the brain and spine. Almost 95% of tumors occur outside of the brain. We noticed that head and neck tumors in skin cancer samples that expressed these markers also had reduced functional status, meaning they have less electrical conduction. They also express proteins associated with nerve injury and neurodegeneration. Moreover, all of these factors also are associated with a poor response to cancer treatment.
What causes this nerve degeneration?
We usually don’t see these markers outside of the central nervous system, so it’s interesting to understand what it is about cancer that causes nerves to have these characteristics because they are typically protected against injury.
One explanation might be that tumor cells directly cause changes to the surrounding nerves by leaving them less oxygenated or raising the acidity level, for example, causing injury to the nerve that can lead to breakdown.
We’ve also seen cancer cells invading and physically crawling along the nerves, using them as highways to spread and metastasize. In patients with head and neck cancers, we can see how these tumors navigate from the skin and mouth to the skull base and the brain, deeming them inoperable.
This perineural invasion, as it’s known, leads to a higher risk of a worse prognosis compared to patients with the same tumor and risk factor whose tumors do not invade in this way. Unfortunately, we know it’s an ominous feature needing escalated treatment, and we don’t yet completely understand the biology behind it.
In these cases, the immune microenvironment is suppressed, and there is an enrichment of inflamed cells that normally serve the purpose of maintaining balance. Essentially, these immune and inflammatory responses are pro-tumorogenic and that undermines our ability to treat those patients with immunotherapy. But we can also use these peripheral nerve injuries as a marker and also as a target to try and identify patients who might respond well to treatment.
Is there a way to heal this nerve damage?
Whenever there is nerve injury, whether it’s due to cancer, Alzheimer’s disease or aging, the body’s innate response is to try and fix it. The interferon response is one of the most recognized pathways involved in wound healing and part of that includes the upregulation of type 1 interferons (IFN-1), which are cytokines known to help maintain this balance and promote the nerve to heal itself.
Interestingly, these IFN-1s are upregulated and linked to neuroinflammation in instances of Alzheimer’s Disease. In tumors, we also find this IFN-1 upregulated in the peripheral nerves and we see that it is associated with immunosuppressive inflammatory responses to cancer in the context of nerve injury. So, two things are happening at the same time. One is the cancer, and one is the nerve injury itself. The two responses are inversely correlated, and they interfere with each other. As a result, patients do not get an effective anti-tumor response. That is what we are trying to overcome.
In our studies, we’ve found that prioritizing the antitumor response is the way to improve outcomes. For instance, inhibiting the wound-healing response in lab models while delivering immunotherapy results in overcoming that resistance. And once you remove the cancer, then you can hopefully allow the nerves to repair themselves.
Learn more at MD Anderson's Cancer Neuroscience Symposium on Feb. 28-March 1, 2024.
Related Cancerwise Stories

It is important to recognize and advance our understanding of the nervous system’s contribution to cancer, so we can identify therapeutic targets and improve treatments.
Moran Amit, M.D.
Physician & Researcher