- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (632)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (918)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (322)
- Symptoms (182)
- Treatment (1786)
My life with an ileal conduit
BY Gabe Gelb
3 minute read | Published November 02, 2015
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on November 02, 2015
In 2009, a urologist told me I needed to have my bladder removed to treat my stage IV bladder cancer. When I asked him how many similar operations he'd done, he told me he averaged at least one a month. I knew then that I needed to go somewhere with more resources and experience.
I'm lucky to live in Houston, so I chose MD Anderson. Upon arriving, I learned that my surgeon, Ashish Kamat, M.D., removed more than twice as many bladders and prostates each week. That was a number I felt much more comfortable with.
My bladder cancer surgery
I'm optimistic by nature, so I wasn't worried about the surgery. After the procedure, I was in pain for a few days, but my philosophy was "This too will pass." And it did.
The day nurses were wonderful and quickly had me walking around. I spent a week total in my hospital room, and several weeks recovering at home, but was soon back to work. The first day out of the house, I was only able to walk for one block. But after a week or so, I began to walk briskly around my neighborhood.
Life with an ileal conduit
I now have an ileal conduit urinary diversion, which allows me to urinate after having my bladder removed. During the surgery, my doctors re-routed a section of my small intestine to connect to my kidneys. It drains into a detachable pouch attached to my abdomen to get rid of the urine. For the most part, I'm living a normal life. Best of all, the bladder cancer has not returned.
A few months after my surgery to create the ileal conduit, someone at MD Anderson offered to connect with me a survivor who'd had the same procedure. I don't remember what that gentleman and I discussed, but I do recall feeling tremendously encouraged that he was there to tell me about it 10 years after his surgery.
I've tried to pay it forward by volunteering with myCancerConnection -- MD Anderson's one-on-one patient support program -- and speaking with patients considering an ileal conduit or to those who are in the hospital after the procedure.
Advice for coping with ileal conduit
Whenever I speak with other bladder cancer patients, I encourage them to ask lots of questions before an ileal conduit urinary diversion. My wife and I faced several issues regarding the weekly replacement of my pouch, and I wish I had known more about what to expect from the beginning. The good news is that MD Anderson has a Wound, Ostomy and Continence Clinic where terrific nurses are experienced in all aspects of post-surgery matters. If you have a similar surgery, I encourage you to visit this clinic before you land on the operating table. I also suggest you stop by afterwards.
I also encourage patients to take advantage of all of the people and resources that MD Anderson has to offer. MD Anderson's surgeons, radiologists, nurses, physician assistants and technologists saved my life. I've been cancer-free for six years and am eternally grateful. MD Anderson consistently ranks as one of the top cancer centers in the country, and stories like mine are the reason why -- at least in my book.
Related Cancerwise Stories
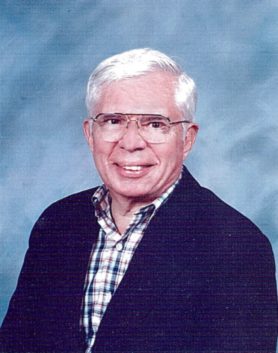
My philosophy was 'This too will pass.' And it did.
Gabe Gelb
Survivor