- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (66)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (68)
- Brain Metastases (28)
- Brain Tumor (230)
- Breast Cancer (718)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (154)
- Colon Cancer (164)
- Colorectal Cancer (110)
- Endocrine Tumor (4)
- Esophageal Cancer (42)
- Eye Cancer (36)
- Fallopian Tube Cancer (6)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (6)
- Kidney Cancer (124)
- Leukemia (344)
- Liver Cancer (50)
- Lung Cancer (288)
- Lymphoma (284)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (98)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (170)
- Pancreatic Cancer (164)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (144)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (236)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (60)
- Testicular Cancer (28)
- Throat Cancer (90)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (78)
- Vaginal Cancer (14)
- Vulvar Cancer (18)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (24)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (230)
- Epigenetics (6)
- Fertility (64)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (124)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (898)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (404)
- Survivorship (322)
- Symptoms (184)
- Treatment (1776)
My kidney cancer treatment before and during the COVID-19 pandemic
4 minute read | Published April 20, 2020
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on April 20, 2020
I was first diagnosed with kidney cancer in spring 2019. I had a chest X-ray because I’d recently quit smoking. My lungs were OK, but the scan caught a tumor on my kidney. Dr. Christopher Wood cut out the baseball-sized tumor with clean margins, and I didn’t worry about anything for another year.
In March 2020, I learned the cancer, renal cell carcinoma, had returned and spread to my spine. This time, everything has been very different, from my treatment to all of the precautions MD Anderson has put in place to protect patients and employees from the novel coronavirus, COVID-19.
New coronavirus precautions make MD Anderson safe for patients
Last year, when I was facing my kidney cancer diagnosis, I brought my wife to appointments. She would listen, ask questions, and we could talk to each other. I had someone to lean on.
But, right now, MD Anderson isn’t allowing patients to bring visitors to appointments in order to reduce the spread of COVID-19. Everybody at MD Anderson is wearing masks, and you have to answer COVID-19 screening questions at the designated entry points.
Having to go through all of my tests and listen to the doctor alone is scary. But I’ve got to hand it to MD Anderson for being proactive and making the hospital a safe place for patients like me. It’s just amazing to see such a large institution so ready, like a well-oiled machine.
How I’m staying connected with my family despite COVID-19 precautions
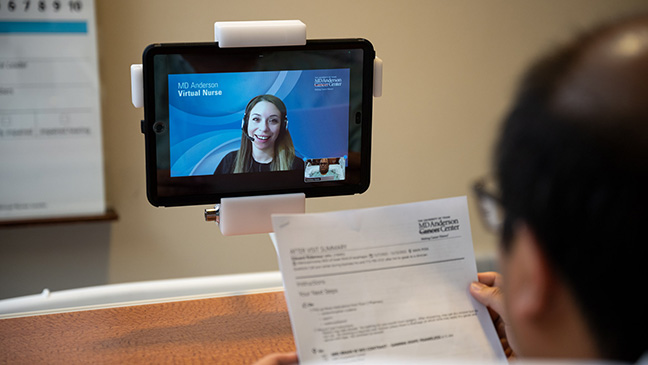
MD Anderson has offered many different ways to help us patients stay connected to our loved ones during appointments during the COVID-19 pandemic. If you wanted to do a video call, you certainly could.
But I’ve been using audio notes on my phone to record my doctor’s appointments. I can bring home the recording, sit at the table and play it for my family. It’s been helpful for me because the doctors give you so much information, it’s easy for some of it to fall through the cracks. When I can just play it back and have my wife hear exactly what came out of the doctor’s mouth, that eliminates any questions.
My second kidney cancer treatment: radiation therapy and targeted therapy
After my first diagnosis, the only treatment I had was surgery called a partial nephrectomy. Dr. Wood removed a third of my kidney and my results were negative. As far as I was concerned, the cancer was gone. I recovered easily and quickly got back to my normal life.
When the cancer came back in my spine, my doctors recommended three sessions of a high-dose radiation therapy called stereotactic body radiation therapy, followed by at least 12 weeks of CABOMETYX®, a targeted therapy pill. While I was lying there with the radiation machine rotating around me, I couldn’t feel anything, but I had faith that the light was finding the cancer.
A surprise bell ringing to mark the end of radiation therapy
I finished my last radiation treatment on April 7, 2020. I’d heard other patients ring the bell, and I thought it meant you were cancer-free.
I didn’t know it was a tradition to ring the bell at the end of radiation treatment, but it made me feel really good to do it. There’s just a wonderful energy that comes out of ringing the bell that resonates with everybody. Afterwards, I wanted to give my radiation oncologist Dr. Chad Tang a hug, but social distancing meant I had to resort to an elbow bump.
It was strange to stand there without my family but with Dr. Tang and the radiation techs, as we all wore masks. We were all laughing and smiling, but you couldn’t see it! I couldn’t do anything but make a joke about it.
Faith in the face of uncertainty
Now I’m in a holding pattern for several weeks until I go back for scans to see how the tumor responded to the targeted therapy drug and radiation therapy. That gray area is the hardest part.
But I have a lot of faith. My cancer was discovered by accident, and I’m fortunate to have a world-renowned cancer center 10 minutes from my house. There’s only one place to go if you’re dealing with cancer. The specialists at MD Anderson do nothing but cancer all day, every day, so I know there’s no better place for me to be.
Learn about precautions MD Anderson is taking to protect patients and employees from COVID-19.
Related Cancerwise Stories

I know there’s no better place for me to be.
Higdon Compton
Survivor