- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (96)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (630)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (916)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (320)
- Symptoms (182)
- Treatment (1786)
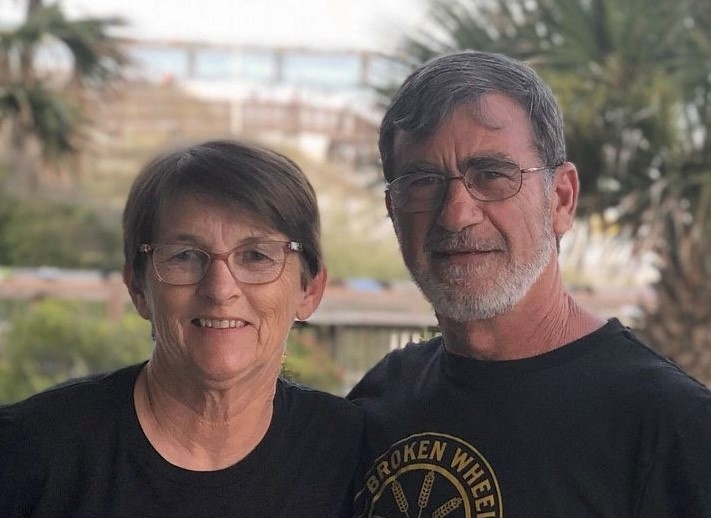
Multiple myeloma survivor grateful CAR T cell therapy clinical trial gives her another option
6 minute read | Published October 22, 2020
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on October 22, 2020
When Trena Robertson’s left hip began aching, she visited an orthopedic specialist in Baton Rouge, Louisiana, her hometown.
“The doctor said I might have arthritis,” Trena recalls. “He prescribed some pain and anti-inflammatory medications, but they didn’t help.”
Little did Trena know that her painful hip was not arthritis, but instead was a symptom of multiple myeloma, a blood cancer that develops in the bone marrow where blood is made. A year would pass before she would be diagnosed with the disease.
As Trena’s pain worsened, she began limping. Navigating the long hallways in the school where she worked as a speech therapist became increasingly difficult.
“I was holding onto walls, trying to walk from one end to the other,” she recalls.
By the time the school year ended, Trena’s entire body was in pain.
“My yearly physical exam was coming up,” she says, “and I was just holding on for that appointment. I needed to understand what was happening with my body.”
A multiple myeloma diagnosis
Bloodwork ordered by her family doctor pointed to possible lupus, a connective tissue disorder that runs in Trena’s family.
Her doctor referred her to a rheumatologist. But it turns out Trena didn’t have lupus. After “undergoing more medical tests than I’d ever had in my life,” the rheumatologist told Trena he was 99% certain she had multiple myeloma.
“I'd never heard of it,” Trena says, “but I knew enough about medicine to recognize that the suffix ‘oma’ usually means cancer.”
The rheumatologist referred Trena to an oncologist who ordered a bone marrow biopsy. The results left no doubt. Not only did Trena have multiple myeloma; the cancer had also taken over 90% of her bone marrow.
The doctor explained that multiple myeloma weakens the bones and increases the risk of fractures. Trena had multiple small breaks in bones throughout her body, in various stages of healing.
“I finally had an explanation for my pain,” she says.
Multiple myeloma is incurable, but treatable, the doctor explained. Many patients do well for years at a time before needing to return to the hospital for additional treatment. She warned Trena that treatment would be intense, and would last about a year.
“With only three days before the start of the new school year, I notified my principal that I needed to take a year-long leave of absence,” Trena says.
Multiple myeloma treatment: chemotherapy plus a targeted therapy
The oncologist prescribed an oral chemotherapy called lenalidomide and a targeted therapy called bortezomib, which is injected just under the skin of the abdomen.
Bortezomib targets particles inside myeloma cells called proteasomes, which act like little garbage disposals by digesting unneeded or damaged proteins inside the cells. Bortezomib targets these proteasomes, and blocks them from digesting and discarding the proteins. The proteins build up inside the myeloma cells, and the cells die. All cells contain proteasomes, but myeloma cells are more dependent on proteasomes than normal cells.
Trena’s doctor warned that the two-drug combo, while effective, would have an unwanted side effect: Healthy blood cells would also be damaged and die along with the cancer cells. After finishing the medication, Trena would need a stem cell transplant to replenish her bone marrow with immature stem cells taken from her own body. These would quickly mature into healthy blood cells.
The doctor urged Trena to make an appointment at MD Anderson, one of the world's largest stem cell transplant centers.
Next step: Stem cell transplant
At MD Anderson, oncologist Krina Patel, M.D., explained that she would work with Trena’s hometown oncologist to coordinate her care.
Together, the two doctors agreed to step up the frequency and dosage of Trena’s medications.
Two months later, her myeloma cell count had dropped low enough to start the next step of her treatment: an autologous stem cell transplant, which would use her own stem cells for treatment.
Trena began taking a special medication called Neupogen that "tricks" the bone marrow into overproducing stem cells. She'd need 5 million for her transplant. Instead, she produced over 18 million.
“I’ve always been an overachiever,” she says.
After undergoing high-dose chemotherapy to kill any remaining cancer cells, Trena received her stem cell transplant Dec. 12, 2018. Much like a blood transfusion, the cells were delivered intravenously. The procedure lasted only 30 minutes.
“I was awake and aware,” she says. “It was completely painless. I felt nothing.”
Stem cells are smart, Patel explains. After they’re infused into the bloodstream, they find their way back to the bone marrow and get to work.
“Remember, when the stem cells arrive in the bone marrow, things are in bad shape – almost all of the old marrow cells have been killed by the chemotherapy,” Patel explains. “The stem cells start working immediately to produce new blood cells. Within one to two weeks, those new cells are mature enough to work correctly.”
Trena recovered with no complications, and was pleased with the result.
“Before my transplant, I was using crutches and a wheelchair to get around because I was so weak,” she says. “By the time I came home, I was walking on my own and doing well. School was about to start, and I was excited to go back to work.”
Another treatment option: CAR T cell therapy clinical trial
But two months later, Trena relapsed.
“The myeloma figured out how to get around the stem cell transplant,” Patel told her. “But we have another option.”
A new clinical trial for relapsed multiple myeloma had recently been approved by the Food and Drug Administration, and was now underway at MD Anderson and four other cancer centers throughout the country.
The clinical trial was testing a relatively new cancer treatment known as CAR T cell therapy, which was already being used to treat some people with relapsed leukemia and lymphoma. The therapy changes a patient’s own disease-fighting T cells so they’re able to recognize and attack cancer.
Here’s how it works: Patients’ T cells are extracted from their blood and sent to a lab to be genetically engineered. In the lab, scientists modify the T cells so they produce a protein (called a receptor) that recognizes another protein (called an antigen) on the surface of cancer cells. This allows the genetically altered T cells to identify and attack the cancer. These specially engineered T cells are then multiplied by the hundreds of millions in the lab, and infused back into the patient to fight the cancer.
Patel, who leads the MD Anderson arm of the clinical trial, urged Trena to join.
“Sign me up,” Trena agreed. “What do I have to lose?”
She took another leave of absence from work and repeated the same bortezomib, lenalidomide and high-dose chemotherapy regimen as before. But this time, instead of stem cells, she received an infusion of her own amped-up, cancer-fighting T cells.
Careful monitoring and treatment
Ten months later, Trena is back at work – virtually for now. Her scans no longer show any signs of cancer. Patel says this doesn’t mean the cancer is gone.
“Multiple myeloma is currently an incurable disease,” she explains. “When you're in partial remission, a few cancer cells still remain in your body. Treatments can't kill every single cancer cell, but there are so few that tests can’t detect them.”
The goal in managing multiple myeloma, Patel says, is to stay one step ahead of the disease with careful monitoring and treatment as needed.
Trena undergoes monthly blood screenings in Baton Rouge, and sees Patel for follow-up appointments every three months in Houston. Managing multiple myeloma is a lifelong commitment, Patel says.
That’s fine with Trena.
“If it gives me the best shot at long-term remission,” she says, “I’m all in.”
Request an appointment at MD Andreson online or by calling 1-844-617-3459.
Related Cancerwise Stories

I'm all in.
Trena Robertson
Survivor