- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (294)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (96)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (630)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
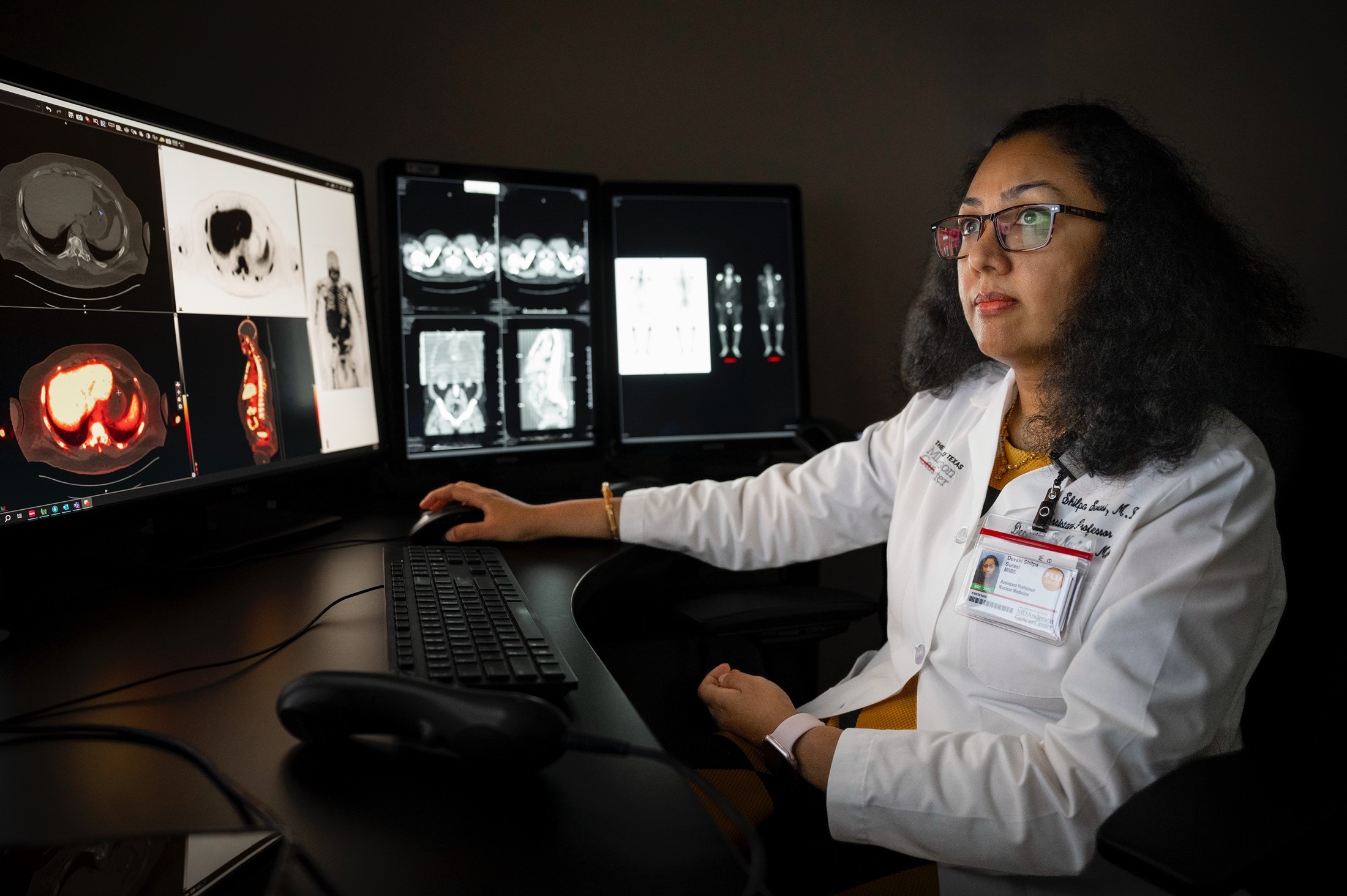
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
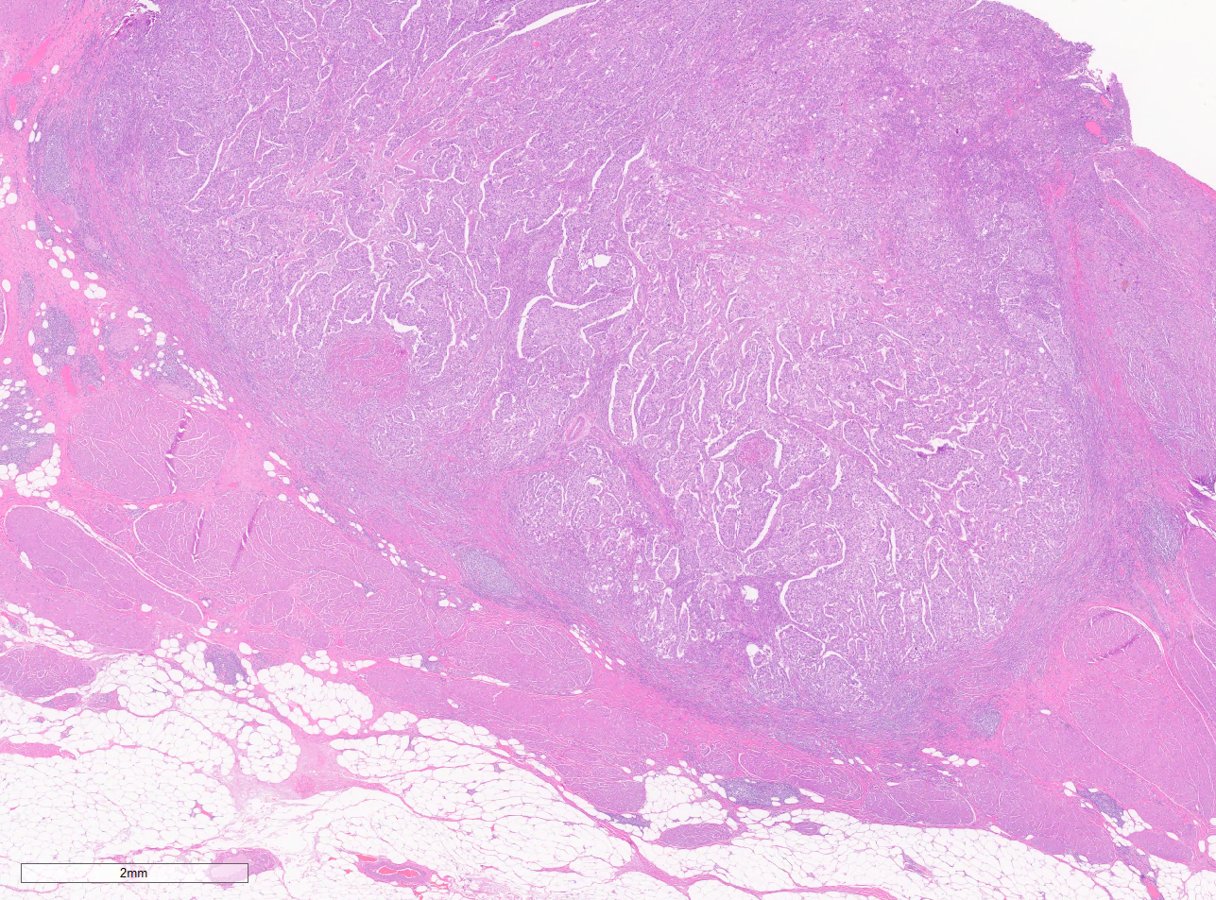
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (912)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (320)
- Symptoms (182)
- Treatment (1786)
Q&A: Minimally invasive surgery for cancer patients
BY MD Anderson
5 minute read | Published July 30, 2010
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on July 30, 2010
Just a few years ago, most surgeries were "open," or invasive, procedures in which a surgeon made a large incision while the surgery went on. Surena Matin, M.D., associate professor in the Department of Urology and medical director of the MINTOS (Minimally Invasive and New Technology in Oncologic Surgery) Collaborative Group, discusses newer, minimally invasive techniques and how they've changed the standard of care for certain types of surgery at MD Anderson.
What is minimally invasive surgery?
In general, minimally invasive surgery means any technique that aims to minimize the trauma of traditional surgery. Practically speaking, we're usually referring to endoscopic, laparoscopic or robotic techniques.
Endoscopic techniques generally refer to any type of procedure that allows the surgeon to view the inside of a body cavity or organ through an existing opening -- for example, diagnostic procedures like colonoscopies.
Laparoscopic also called band-aid or keyhole, surgery refers to operations in the abdomen performed through small (0.5-1.5 cm) incisions. A laparoscope (essentially a miniature camera) is used to guide the surgeon, and a light helps illuminate the area.
Fairly new, robotic surgery uses a sophisticated robotic system to perform laparoscopic surgery. The surgeon, seated at a console across the room, wields instruments as he or she watches a video monitor of the surgical area.
The technology actually allows the surgeon to even be miles away, a concept called "telesurgery". This has been tested and shown to be possible with simple operations but is not yet routinely done as there are many technical, legal, financial and ethical considerations that have not yet been addressed.
What skills does a surgeon need to perform these techniques?
Surgeons performing minimally invasive procedures need expert hand-eye coordination and the ability to work in a small area with a limited view and without tactile clues. The biggest challenges with laparoscopy include working in a three-dimensional field while having only a two-dimensional view (the TV monitor) and the lack of dexterity with typical straight laparoscopic instruments. Robotic technology addressed both those constraints by providing a 3-D view and instruments with dexterity.
How long have these techniques been around?
It's been more than two decades since the first gallbladder was removed and two decades since the first kidney was removed laparoscopically. Robotic techniques have been performed for fewer than 10 years, and as a routine practice in most centers, less than five to seven years.
What are the benefits, in general, of minimally invasive techniques?
Generally there is less pain, less bleeding, less scarring, a shorter hospital stay and recovery time. But, this really depends on the type of operation and the disease being managed, and just as important, on the surgeon and his or her experience. In some cases, minimally invasive techniques offer no clear benefit.
For patient Adeline "Gail" Smith, minimally invasive surgery was the best answer. The kidney and entire ureter down to the bladder, including a portion of the bladder that surrounds the ureter, needed to be removed. The old-fashioned approach required one very long incision or two separate incisions. With minimally invasive surgery, she experienced less scarring, pain and loss of blood, plus she could go home sooner.
What are the risks of this surgery?
We have to remind patients that even though the incisions are small, the surgery is no less risky. In fact, in inexperienced hands or with more complex cases the risks may even be higher than traditional surgery. So the typical risks of major surgery are still present. Punctures, perforations or injury to nearby organs, infections and anesthesia complications are a few of the risks. And patients who've had previous surgeries might be at higher risk for complications.
We work very hard at minimizing risk. The fact is, however, that we cannot eliminate risk. Also, what most people don't realize is that health care efforts are only part of the equation. Patients play a big role in minimizing risk by quitting smoking, improving their exercise capacity, losing weight and other "modifiable risks."
Which procedures lend themselves to this technique?
In urologic cancer surgery, feasibility and safety has been shown for:
- Kidney cancer
- Laparoscopic radical nephrectomy, removal of a kidney
- Nephroureterectomy, removal of a kidney and its ureter
- Robotic partial nephrectomy, removal of part of the kidney
- Prostate cancer
- Robotic prostatectomy, removal of the prostate
- Bladder cancer
- Robotic cystectomy, removal of all or part of the bladder and lymph nodes
In each of these cases, we are also doing aggressive lymph node removal when necessary. With penile cancer, we are evaluating the role of endoscopic inguinal lymph node removal. This technique removes the possibly involved lymph nodes -- the nodes that lymphatic fluid moves to first -- to see whether cancerous cells are present. The hope with this procedure is to minimize the incision size, which has clearly been associated with high wound complications so that the patient is spared complications.
In orthopedic surgery, arthroscopic techniques, which address problems inside of a joint like the knee, shoulder, etc., have been used for a number of years. Minimally invasive techniques are also well established or gaining ground in gynecological, thoracic and cardiac surgeries. There are very promising developments in head and neck surgery and endocrine surgery. Even our plastic surgeons are doing complicated reconstructions after major resection of head and neck cancers.
How has the use of these techniques grown at MD Anderson?
Based on 2009 data, we've quadrupled our minimally invasive procedures since 2001 and tripled them since 2004. We now do over 3,200 a year, if you look at all kinds of minimally invasive procedures. Since 2004, when we first started tracking this more carefully, and until the end of fiscal year 2009, we had done 13,275 procedures.
This growth is mostly seen in urologic oncology and gynecologic oncology, but as mentioned above many other specialties are learning from one another and applying these techniques to their fields. It's a growing trend as cancers are detected earlier, as minimally invasive surgery lends itself to treatment of early-stage disease. The techniques are also sometimes used for diagnostic purposes.
Is minimally invasive surgery preferable for the procedures listed above?
Sometimes minimally invasive procedures are not better than the open counterpart in every respect. There are trade-offs, just as in everything we do, including when we decide not to operate.
One procedure may be associated with a shorter recovery time, but it may come at the cost of a slightly higher risk of a particular complication. Sometimes the cancer is not perfectly suited for a minimally invasive procedure, but minimally invasive is what the patient really wants; we need to make sure those patient expectations are realistic and based on facts, not hopeful wishes. In these cases when there are choices and resulting trade-offs, patients play an important role -- with the surgeon as guide -- in determining what's important to them and what their priorities are.
Related Cancerwise Stories