- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (66)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (28)
- Bladder Cancer (68)
- Brain Metastases (28)
- Brain Tumor (228)
- Breast Cancer (716)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (154)
- Colon Cancer (164)
- Colorectal Cancer (110)
- Endocrine Tumor (4)
- Esophageal Cancer (42)
- Eye Cancer (36)
- Fallopian Tube Cancer (6)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (6)
- Kidney Cancer (124)
- Leukemia (344)
- Liver Cancer (50)
- Lung Cancer (288)
- Lymphoma (284)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (98)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (170)
- Pancreatic Cancer (166)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (144)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (236)
- Skin Cancer (294)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (60)
- Testicular Cancer (28)
- Throat Cancer (90)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (78)
- Vaginal Cancer (14)
- Vulvar Cancer (18)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (622)
- Complementary Integrative Medicine (24)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (226)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (122)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (64)
- Palliative Care (8)
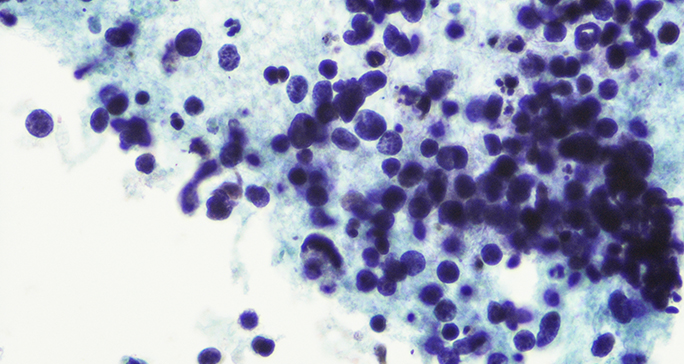
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (888)
- Research (388)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (602)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (404)
- Survivorship (322)
- Symptoms (186)
- Treatment (1770)
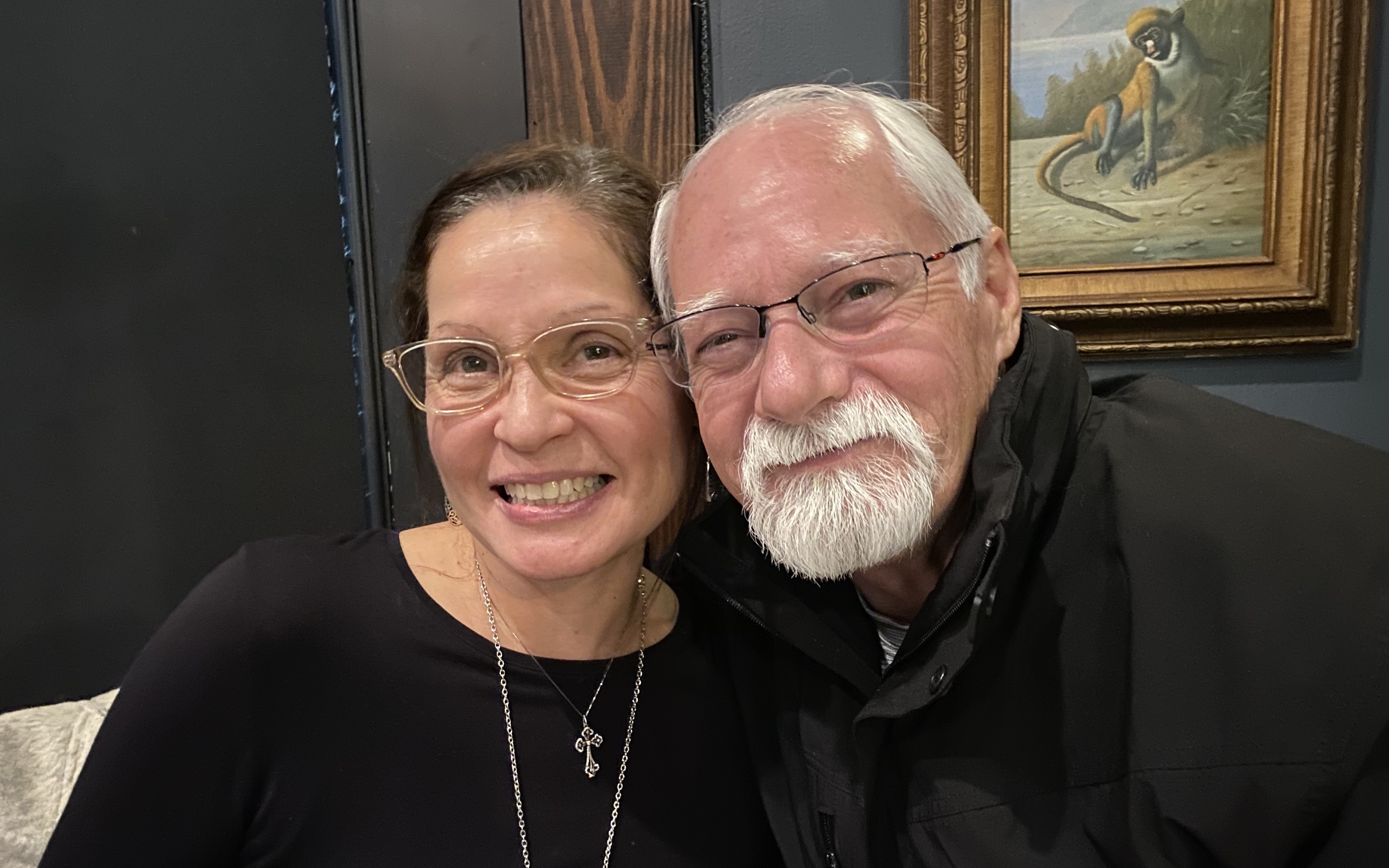
Is a clinical trial right for me?
BY Julie Nagy
4 minute read | Published June 01, 2023
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on June 01, 2023
Clinical trials are research studies that evaluate a new drug or treatment to make sure that it is safe and effective for patients.
“Clinical trials are essential to be able to identify better treatments for patients with all tumor types,” says Funda Meric-Bernstam, M.D., chair of Investigational Cancer Therapeutics. “It’s also an opportunity for patients to access otherwise unavailable treatments and to contribute to better outcomes for future patients.”
So, how can you find out if a clinical trial is right for you? Use our answers to these common questions about clinical trials to help you have a more informed conversation with your care team.
What kind of clinical trials are there?
Many clinical trials are for treatments tailored specifically for a certain disease or condition to ensure the most efficient approach.
“We have over 1,000 active trials at MD Anderson at any given time, which means there is a very high likelihood of identifying a trial that would be a good fit for a patient,” says Meric-Bernstam.
How do I qualify for a clinical trial?
Clinical trials are available for patients at all stages of disease. You need to meet certain requirements, such as having the appropriate condition or biomarkers which are being examined. Additionally, some drugs have known side effects that could be harmful to certain people. This is why every clinical trial has a protocol with strict inclusion and exclusion criteria that are usually based on:
- specific age ranges
- type of disease (for instance, type of cancer and extent of cancer spread)
- prior treatment history
- chronic health conditions
- pregnancy or intent to become pregnant
- liver or kidney function
- medications you take that might interfere with the trial drug
- other considerations that vary depending on the treatment being tested
These inclusions and exclusions are one of many ways in which clinical trials prioritize your safety. It is important to talk openly and honestly with your care team about your medical history because there may be something about the treatment that might negatively affect your body. In turn, your care team will inform you of any potential risks or known side effects so that you can make a fully informed decision.
“It is very important for us to be open about what is known and what is not known about a treatment so that patients can be informed of their options,” Meric-Bernstam says.
What are the different phases of clinical trials?
For a drug or treatment to be approved for use as standard treatment, it must pass through several clinical trial phases. Each phase has a different purpose.
Phase I clinical trials are usually the first time an experimental drug or a new drug combination is given to a human. During this phase, researchers are trying to figure out the correct dose, or how much of the drug can be given safely. Phase I clinical trials usually only have between 15 to 50 patients, and doctors and nurses are monitoring very closely for any signs that a drug or drug combination might have unexpected side effects.
Phase II clinical trials usually enroll fewer than 100 patients to test if the established dose of the treatment shows signs that it works.
Phase III clinical trials enroll hundreds to thousands of patients to compare the standard treatment to the new experimental treatment to see if it works better than what is currently available. In some Phase III trials, neither the patients nor the doctors know if a participant is receiving the experimental treatment or the standard of care. This is to avoid any potential bias or expectations.
After Phase III clinical trials, the Food and Drug Administration (FDA) reviews the results and decides whether to approve the new treatment. If it gets approved, the drug becomes available for people who weren’t on the trial. The drug can even be tested to see if it’s effective in treating other diseases.
Related: 5 things to know about the FDA approval process
Are clinical trials safe?
While you’re on a clinical trial, a team of doctors and clinical staff will closely monitor you to make sure you are safe at all times. Your care staff will check your lab results constantly to see if the treatment is working as expected and make sure you don’t experience unintended side effects. They also will provide contact information to reach someone who can address your concerns at any time.
Remember that participation in a clinical trial is completely voluntary. You can withdraw your consent at any point and for any reason.
Are clinical trials right for me?
Talk to your care team to find out if you are a good candidate for a clinical trial.
It is important to consider your standard treatment options and the expected results based on your circumstances. Your doctor or specialist is your best resource for understanding all the potential risks and outcomes that may come with a given trial. They can help guide you to make the decision that’s right for you.
Your eligibility for certain phases of trials may vary based on your condition. You should weigh potential risks and side effects as well as additional tests, visits and travel requirements.
Clinical trials are not for everyone, but they can expand your treatment options if you meet the criteria and want to participate. When it comes down to it, your doctor or specialist is the best resource for determining whether or not you would be a good candidate. Their main priority, after all, is making sure you have access to the best possible treatment options that can be safely tailored to your needs.
Request an appointment at MD Anderson online or by calling 1-877-651-1567.
Related Cancerwise Stories

We have over 1,000 active trials at MD Anderson at any given time, which means there is a very high likelihood of identifying a trial that would be a good fit for a patient.
Funda Meric-Bernstam, M.D.
Physician & Researcher